“Many people mistakenly believe that Alzheimer’s disease is a “natural” outcome of aging- this is simply not true. Although advanced age is a risk factor for the disease, it is not an expected outcome of aging. If you are worried that you might be showing signs of Alzheimer’s disease, or you are reading this because you are concerned about someone you care about, it’s important to know that early diagnosis can help slow progression of the disease. It’s important to get an early diagnosis so that treatment can start early”.
-Dr. Bella Zimilevich, MD
What is Alzheimer’s disease?
Alzheimer’s is the most common form of dementia. Dementia is a condition that causes memory loss and a decline in cognitive functioning. Alzheimer’s disease is the most common form of dementia, accounting for somewhere between 50 to 80% of cases of dementia.
What are the risk factors for Alzheimer’s disease?
Age is the single greatest risk factor for the development of Alzheimer’s. Notice that I did not say that aging causes Alzheimer’s (younger people are sometimes diagnosed with Alzheimer’s, but far less often than older individuals), but Alzheimer’s does become more common as age advances. Most people diagnosed with Alzheimer’s are 65 years of age or older.
Heredity is known to be a factor in Alzheimer’s disease. If you have a close family relative (parent, sibling or child) with the disease, your risk is higher than someone who has no family history of the disease. Scientists have identified genes that are implicated in Alzheimer’s disease. Some genes raise your risk of of developing Alzheimer’s, while others almost guarantee that you will develop Alzheimer’s. However, it’s important to know that the type of Alzheimer’s that is passed down through generations of the same family is rare, accounting for only about 5% of all cases of Alzheimer’s disease.
Most experts believe that there is no single “cause” of Alzheimer’s. Rather, it is thought that Alzheimer’s develops from a combination of genetic factors and other risk factors. You can’t change your age or your genes, but scientists believe there are other factors that may come in to play that you may have some control over, such as:
- traumatic brain injury- there is some evidence to suggest that patients who have experienced trauma to the brain are at higher risk of developing Alzheimer’s later in life. It’s not a good idea for anyone, regardless of age and risk of dementia, to expose their brain to trauma, so wear a helmet while participating in sports and wear your seatbelt while driving or riding as a passenger.
- heart, lung and cardiovascular health- we know that the brain is nourished with oxygen and other nutrients, so it stands to reason that anyone with an issue affecting blood supply and blood oxygenation may be at higher risk of developing dementia. Control your weight, blood pressure, cholesterol level and blood glucose levels and avoid excessive alcohol use and smoking. In addition, eat a heart healthy diet and try to exercise regularly. All of these can help to keep your heart and lungs (and thus your brain) healthy.

What signs and symptoms might signal the development of Alzheimer’s disease?
The following are some symptoms/signs associated with Alzheimer’s:
- frequent problems finding the right word when writing or speaking
- misplacing things
- showing poor judgement
- withdrawal from people, social activities or work
- personality/mood changes
- memory loss that affects ability to function
- difficulty in performing tasks that were once easy
- memory loss
- difficulty with problem solving/planning
- confusion regarding time and place
- difficulty interpreting visual images or spatial relationships
We may all have difficulty with an item on this list from time to time. People with Alzheimer’s may have difficulties with many of the items on this list on a regular basis, and these difficulties tend to get worse over time. There are seven stages of Alzheimer’s, ranging from stage 1 (no impairment) to stage 7 (very severe decline).
What can I expect if I come to see you (or I bring my loved one to see you)?
You can expect that I will treat you (or your loved one) with respect and dignity. I am an internal medicine physician and I specialize in geriatrics, which means I have specialized training in caring for older individuals. Most importantly, I care and I want to help you or your loved one if you are concerned about Alzheimer’s, as I know just how scary the symptoms can be, and what a diagnosis of Alzheimer’s disease means.
First of all, I will want to take a detailed medical history. I will want to know about past and present medical problems, past surgeries, current medications and allergies. I will also want to perform a thorough physical exam, which means that you will be asked to change into a gown. I will assess you completely from head to toe. I will also do a neurological examination to see if there are balance and/or gait problems, visual problems or other neurological issues. I may also perform mental status testing, which involves testing of memory, recall and other cognitive functions. Lastly, I may order blood work, brain imaging exams or other diagnostic tests if I feel that symptoms are consistent with Alzheimer’s disease. If I order tests, I will tell you why I think the test is necessary and what I think the test will rule out or tell me. It’s important to know that other diseases and conditions can cause some of the symptoms of Alzheimer’s, and that these conditions may be completely reversible, so it is important to rule them out.
Once I have all of the information I need, we’ll discuss the results and decide on a plan of care. If you, or your loved one, have Alzheimer’s disease it is important to know that, although the condition can’t be cured, there is treatment available that can slow disease progression. Medications can help with memory, sleep disturbances and other symptoms of the disease. It’s also important to know that there is a lot of research going on regarding Alzheimer’s disease, and new knowledge is coming forward all the time.
If you are concerned that you may have Alzheimer’s disease, or you worry that a loved one is showing signs, make an appointment to see me. The sooner you come in, the sooner you will have an answer. If Alzheimer’s is the reality, treatment can begin immediately, which can help to slow disease progression and symptoms.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“It may not be a pleasant subject to discuss , but diarrhea is a common problem that is sure to affect everyone at one time or another. Numerous health conditions can cause diarrhea. Most of the time, diarrhea is caused by a dietary indiscretion or a viral illness and is short-lived, but for some diarrhea can be a symptom of a more serious condition. If your diarrhea last longer than a few days, you should make an appointment to come in and see me”.
-Dr. Zimilevich, MD
What is diarrhea?
Like constipation, diarrhea may mean different things to different people. The frequency and consistency of bowel movements is highly individual. Diarrhea can be described as stools that are more frequent and looser/more watery in consistency.
What symptoms might occur along with diarrhea?
Along with frequent and loose/watery stools, you might also have:
- abdominal pain/cramping
- bloating
- low-grade fever (if your diarrhea is caused by a virus)
- nausea/vomiting
What causes diarrhea?
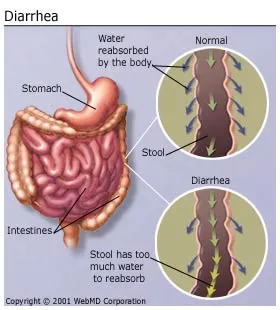
Diarrhea is the result of increased bowel transit time- in other words, food and fluids pass too quickly through your bowel. When transit time is normal, your body pulls water from your bowels, leaving a semi-solid stool to be passed. When stool passes through so quickly that little water is absorbed, diarrhea is the result.
There are numerous conditions that can cause diarrhea, including:
- viral illness– we’ve all experienced viruses that cause diarrhea along with nausea and vomiting; these viruses generally cause illness for 1 to 3 days
- bacterial illnesses- bacteria in water or food may cause diarrhea; you may also have fever, abdominal pain and blood in your stool
- medication– antibiotics often cause diarrhea, as do many other medications (if you think your medication is causing diarrhea, you should schedule a visit)
- irritable bowel syndrome (IBS)- IBS is a functional bowel disorder (meaning that nothing is wrong with the bowel structurally); IBS may cause diarrhea alone, constipation alone, or alternating constipation and diarrhea. Abdominal bloating is also a feature of this common disorder
- lactose intolerance– people who lack the enzyme required to break down the sugar in milk may suffer from bloating, cramping and diarrhea after consuming dairy products
- surgery- if you have had abdominal surgery, you may experience diarrhea transiently or permanently, depending on the procedure that was performed
- celiac disease (gluten intolerance)– in this disorder, people are unable to digest gluten, which is found in many foods
- Crohn’s disease/ilcerative colitis– these are inflammatory bowel disorders that can cause diarrhea, blood in the stool, abdominal pain and other symptoms
- parasites– parasitic infections (often picked up while traveling) may cause diarrhea
These are just a few of the causes of diarrhea- there are many more.
How do I know if my diarrhea is serious?
It can be difficult to know when your diarrhea is bad enough that you should make an appointment to see me. Generally speaking, you should make an appointment if:
- you have a high fever for more than a day
- you are passing blood in your stool (may be bright red or tarry black stools)
- you are dehydrated (you feel weak, dizzy, pass very little urine or your urine is dark, your pulse is fast or your mouth is very dry)
- you have severe stomach/abdominal pain
- you have had frequent diarrhea for more than 48 hours
- you have an underlying health condition such as diabetes, heart disease or other serious illness
What can I expect when I come in?
When you come to see me with diarrhea, I will ask about your symptoms. I will need to know when your symptoms started, whether you have traveled, how frequently you are passing loose or watery stools and what other symptoms you are experiencing (i.e., vomiting, fever, abdominal pain). I will want to know about your past medical history if you are a new patient. I will also need to know if you have any allergies.
I will take your vital signs. Abnormal vital signs, such as low blood pressure and a rapid pulse, may tell me that you are dehydrated. I will need to examine you (you may need to change into a gown for the examination). I will listen you your abdomen and press gently so that I can determine if any area of your abdomen is tender when I press on it. I may also listen to your heart and lungs. I will look for signs of dehydration (dry mouth, sunken eyes).
Depending on my findings and your history, I may order diagnostic tests such as blood work, stool samples, and abdominal x-ray or other tests. I will tell you what I am ordering and why I am ordering a particular test. I will also discuss the results of any test with you, so that we can decide how best to treat you. Treatment will depend on what the problem is.
If you are experiencing diarrhea that has lasted more than a couple of days, especially if your diarrhea is associated with any of the serious signs and symptoms listed above, you should make an appointment to come in and see me as soon as possible. Although you may just have a viral illness, there are many conditions that have diarrhea as a feature.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Suture removal is a simple procedure that can be performed quickly in my office. Although it is an easy procedure, trying to remove sutures yourself is never a good idea, as pieces of stitches can be left behind and infection may occur. If the idea of having your sutures removed makes you nervous, don’t worry- the procedure is not painful and will be over before you know it!”
-Dr. Zimilevich, MD
Repair of the skin is generally achieved by either stitching (suturing) the skin closed or by using staples. If you have sutures or staples, you might be dreading having them taken out. I’m here to assure you that the procedure is quick and virtually painless in experienced hands.
Types of skin closure materials
There are two types of sutures, absorbable and non-absorbable. Absorbable sutures break down eventually (usually within a month or two) and do not have to be removed. Non-absorbable sutures, on the other hand, are used to close external wounds in the skin and must be removed after a period of time.
Staples look just like office staples. They are easy to put in and pose less risk of infection. They may be used to close scalp wounds or operative wounds, but can sometimes leave scarring.
Skin closure tapes are also sometimes used, but it can be difficult to perfectly align the wound edges using skin closure tape, and tape might not adhere very well to areas with lots of body hair or areas that are prone to sweating.
Adhesive agents (skin glue), similar to crazy glue, can also be used to close a wound, especially in children because there is no need to anesthetize the skin prior to gluing. However, skin glue cannot be used on any area of the body where the skin is required to move, such as knees and elbows.
Prior to suture or staple removal
If you have sutures or staples in place, you will have received instructions on how to care for the affected area, such as keeping the area clean and dry for the first couple of days, covering the area with a band-aid if there is bleeding or discharge, watching for signs/symptoms of infection and when to return for removal of your sutures or staples. You will need to make an appointment to come in and have your sutures or staples removed. In general, removal time for specific areas of the body are as follows (you may be given a different timeline):
- arms/legs- 10 to 14 days
- trunk- 7 to 10 days
- joints- 14 days
- scalp- 7 to 10 days
- face- varies from 3 to 7 days, depending on the area of the face

Using sterile forceps and suture scissors for suture removal.
What can I expect during the suture removal procedure?
You will be positioned comfortably so that the area with sutures or staples is easily accessible. The affected area will be cleansed to remove debris and loosen any scar tissue forming. Using sterile forceps, I will carefully pick up the knot of each suture and, using a blade or sterile scissors, I will cut the suture. I will then use the forceps to pull the suture gently to remove it fully intact. You may feel a slight tugging sensation, but it will not hurt. I will continue with each individual suture until all of them have been removed. If you have staples, I will use a special tool that resembles a wire cutter to grasp each individual staple in the center. By squeezing the handles of the tool together, the staple’s edges are bent upwards and the staple can be gently pulled straight up and out. Again, you won’t feel any pain.
Following, I will clean the wound again. I may apply adhesive strips to help hold the wound edges together for a few more days until the wound has strengthened again, or I may apply a bandage to cover and protect the wound. It depends on the size and location of the wound.
After suture/staple removal
Just because your sutures or staples are out does not mean you are off the hook as far as wound care goes! You still need to:
- leave the adhesive strips in place for approximately 5 days, or until they fall off naturally
- keep your wound dry and clean
- protect your wound from trauma for about a month, as your wound will be fragile and prone to splitting open should you suffer an injury in the same area
- protect the area from too much sun
If you need to come in for suture removal, don’t worry- the procedure is quick and painless. Be sure to call and make an appointment to come in for your suture removal well before the due date to ensure that your sutures are not left in too long, as this can make it more difficult to remove them.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Congestive heart failure is a chronic condition that can directly affect quality of life. If you have CHF, you will need to be diligent in caring for yourself, and you will need to partner will a physician who can help you manage your condition to avoid hospitalizations and complications. I would love to be your trusted resource and help you live your life to its fullest potential”.
-Dr. Zimilevich, MD
What is CHF?
Congestive heart failure is a condition that develops after your heart has suffered damage from a heart attack or other condition affecting the heart. In CHF, the heart is weak and is less efficient at pumping blood to other parts of the body. It is also sometimes less able to accept blood back into the heart that comes from the lungs, which accounts for many of the symptoms of this condition. Although there is no cure for CHF, with proper treatment you can live a long and full life; however, attention to your condition and proper medical care is important, which is why you need a doctor who you can trust, one who can help you learn about and manage your condition.
What causes CHF?
Having a heart attack is the most common cause of congestive heart failure. These other conditions can also cause CHF:
- undiagnosed or improperly treated high blood pressure (hypertension)
- disease of the heart valve(s)- leaking or narrowing of the valves
- idiopathic heart muscle disease
- obesity
- diabetes
- myocarditis or endocarditis- inflammation of the heart muscle caused by an infection
- alcohol or drug abuse
- anemia, thyroid disorders and other medical conditions
- high blood cholesterol– over a long period of time
What are the symptoms of CHF?

When you understand what CHF is (the inability of your heart to pump blood properly to the rest of the body or to fill properly with blood returning from the lungs) it is easy to predict the symptoms you might experience:
- shortness of breath- may be severe and may get worse when you lay flat due to excess fluid in the lungs
- bloating or feeling full all the time- excess fluid in the abdomen can cause you to feel uncomfortably full
- feeling tired all the time-lack of oxygen, or poorly oxygenated blood, can make you feel tired
- swelling of the ankles, legs, abdomen or sacral area (base of the spine)- excess swelling is due to the heart’s inability to circulate properly, which leads to fluid accumulation
- sudden weight gain (may be as much as 5 pounds in a week or 2 to 3 pounds in a day or two)- due to fluid accumulation
- coughing or cold symptoms that last far longer than normal- coughing is due to fluid/congestion in the lungs
- increased urination, especially at night- the body attempts to get rid of excess fluid through urination
- loss of appetite- fullness in the abdomen and living with a chronic illness can dull the appetite
What can I expect when I come to see you in the clinic?
If you come to see me in the clinic with any of the symptoms described above, I will want to know how long you have had symptoms and whether you have any of the other symptoms listed above. I will question you closely about your symptoms and what brought you in to see me.
I will need to know about your past medical history, especially if you have had a heart attack in the past or have been diagnosed with another heart condition such as a valve problem. I will need to know what medications you are taking and any allergies you may have. I will also want to know if there is a family history of heart disease.
Next, I will examine you. I may ask that you change into a gown for this part of your visit, as it will be easier to pick up any signs of CHF. I will listen carefully to your heart and lungs for abnormal heart sounds and lung congestion. I will examine your abdomen for any swelling. I will also look at your legs, feet and ankles for signs of swelling. I may obtain your weight as a baseline. I’ll ask about cough, fatigue and increased urination, all of which you may have experienced if you have CHF.
Diagnostic tests can help me make the diagnosis. I may order blood work, an ECG (a heart tracing that tells me about the electrical activity of your heart) and a chest x-ray (can detect an enlarged heart and/or fluid in the lungs). If I feel its necessary I may also order a stress test and/or an echocardiogram, which is an ultrasound of the heart that can tell me a lot about the structure and function of your heart.
I will explain the tests to you, including the reason I am ordering them and what I expect the test to tell me. If any results are abnormal, I promise to explain them to you in terms that you can understand. If necessary, I will refer you to a cardiologist, a physician who specializes in the heart.
How is CHF treated?
Many people with congestive heart failure can be managed with medications, including:
- antihypertensives (medications to lower blood pressure)
- diuretics (medications that help your body rid itself of excess fluids)
- medications such as digoxin, which help the heart to beat more strongly
Some people with severe CHF may require surgery to put in a pacemaker or surgery to unblock clogged arteries. If you need surgery, I can work with you and your surgeon during and after recovery to follow his/her recommendations.
Lifestyle changes are an important part of managing CHF. You may be asked to:
- restrict your daily fluid intake to less than 2 liters a day from all sources
- monitor your blood pressure, pulse and weight regularly at home
- exercise in moderation
- quit smoking
- eat a heart-healthy diet
- increase the fiber in your diet
- decrease the amount of sodium you consume
- avoid excess caffeine and alcoholic beverages
- get lots of rest and sleep
- protect yourself from preventable disease by getting a flu shot and the pneumococcal vaccine
- take your medications on time as prescribed
If you are diagnosed with congestive heart failure, your life will change. With proper treatment, you may find that you feel better and have more energy; however, CHF is a chronic condition that requires careful monitoring for the rest of your life. If you think you might have CHF, or you have already been diagnosed and need a physician who can partner with you to help you lead the best life possible, make an appointment to see me. I can help you manage your condition so that you can enjoy good quality of life.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Sore throats are common, especially during the winter months when many viruses are circulating. Most sore throats caused by a viral infection will not require treatment, but sometimes sore throats are the result of a bacterial infection and antibiotics are needed. If you have a sore throat that is making it difficult for you to eat, drink or talk, make an appointment to come in and see me”.
-Dr. Zimilevich, MD
Although most sore throats (called pharyngitis in medical lingo) are not serious and don’t require treatment except comfort care, some sore throats require treatment with antibiotics. Generally, a sore throat caused by a bacterial infection will produce other symptoms in addition to your sore throat that might prompt you to seek medical care. The tricky part is being able to tell the difference!
Sore throats caused by viral infections
Viral infections, including the common cold, are most common during the fall and winter months when people are indoors and in crowded conditions. Sore throat may be accompanied by a runny nose, mild muscle aches, fatigue and a cough. Symptoms generally subside in 7 to 10 days. Most people with a viral sore throat are able to continue their daily activities and manage their symptoms with rest and over-the-counter remedies.
Sore throats caused by bacterial infections
Approximately 10% of the time, a sore throat in adults is caused by a microorganism called Streptococcus, commonly referred to a strep throat. If you have strep throat, you may feel quite ill. Your sore throat may be so sore that swallowing is very painful. In addition to an extremely sore throat, you may have:
- white patches (pus) visible on the back of your throat
- a fever, which may be high
- enlarged lymph glands in your neck
- little or no cough and runny nose (rhinitis)
- malaise (little energy to do anything, general sense of unwellness)
In addition to strep infection, mononucleosis can also cause an extremely sore throat, fever, and swollen lymph glands. Mononucleosis is caused by the Epstein-Barr virus. Influenza, also caused by a virus, sometimes causes sore throat and can make you feel very unwell.

What can I expect when I come to see you?
When you come in to see me complaining of a sore throat, I will want to know a little about you (if you are a new patient). I’ll need to know about your past medical history, specifically if you have any chronic health problems that can affect immunity. I’ll ask about any allergies you may have in the event that I need to prescribe a medication for your condition.
Next, I will examine you. In addition to looking at your throat to check for swelling, pus and redness, I will look in your ears and listen to your heart and lungs. I may also examine your abdomen (especially if I suspect mono, which can cause your spleen to enlarge). My examination will be focused on your throat, but may be expanded elsewhere, depending on what I suspect the problem to be.
Any of the following is worrisome and should prompt you to make an urgent appointment, as any of the following could be a sign/symptom of a serious problem:
- drooling (inability to swallow saliva or secretions)
- rash associated with fever and sore throat
- swelling that involves the tongue and neck (which could occlude your airway, making it difficult to breathe)
- breathing difficulties
- neck stiffness
- an impaired immune system
I may order diagnostic tests if I feel they are necessary, such as a complete blood count, a chest x-ray or x-ray of the soft tissues of the neck, a rapid strep test or a culture of material from the back of your throat. A rapid strep test can determine in a few minutes if your throat is infected with the streptococcus bacterium.
If I feel that you have a viral sore throat, I will recommend symptomatic treatment, such as rest, plenty of fluids, mild pain relievers and lozenges/throat sprays/oral rinses as necessary. Antibiotics will not be helpful if you have a viral infection and may cause more harm than good.
If I suspect the cause of your sore throat is bacterial in nature, I will prescribe antibiotics such as penicillin, or an alternative antibiotic if you are allergic to penicillin. Generally you will start to feel better within 24 to 48 hours after starting the antibiotic- if you do not start to feel better within 3 days, you should come back in to see me.
If you have a very sore throat, especially if it is accompanied by any of the signs/symptoms listed above, make an appointment to come in to see me. I will be happy to evaluate your sore throat and help you determine the cause and necessary treatment.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Many adults suffer from acne, which can lower one’s self-esteem. If your skin (and your confidence) is affected by acne, I can help. Make an appointment to come in and see me and together we can come up with a plan to banish your acne for good; at the very least, we can improve your complexion substantially and change the way you feel when you look in the mirror”.
-Dr. Zimilevich, MD
What is acne, and what causes it?
Acne is caused by clogging of the skin’s pores. Normally, when skin cells die, they rise to the surface of the pore and are then shed. When your skin produces a lot of sebum (the oil that moisturizes your skin), the skin cells that have died clump together within the pore and become trapped inside. Our skin is colonized by bacteria known as P. acnes; this bacteria can get inside clogged pores, which provide the perfect medium for bacterial growth, which causes the pores to become red and inflamed. When inflammation occurs deep within the pore, a nodule or cyst can form.
Acne is not just pimples (pustules)- many other skin blemishes can form, including blackheads, whiteheads, cysts, nodules and papules. Acne can form on the face, the neck, the shoulders, the upper arms, the chest, the back and the buttocks. Some people have acne in one place only, while others have acne is numerous places. However, facial acne is what concerns most people due to the importance that we place on appearance in today’s society.
Adult acne is more common in women due to hormonal influences; in fact, some women get adult-onset acne during menopause. Acne can be a side effect of some medications and may be caused by certain medical conditions.

In addition to the darkened areas of skin that can occur after acne has healed and the scars that can left behind from cysts and nodules, many people with severe acne suffer from low self-esteem and depression. People with severe acne may be withdrawn and socially isolated because of their appearance or, more accurately, because of the way they feel about their appearance.
What can I expect when I come to see you about my acne?
If you come in to see me because you have acne I will need to take a detailed medical history, particularly if you have new-onset acne. Certain medical conditions, such as diabetes, adrenal disorders and PCOS (polycystic ovarian syndrome, a common female metabolic disorder) can cause or worsen acne. I will also need to know what medications you are taking, in case one of your medications (i.e., steroid medication, seizure medication) is contributing to your acne. If you are a women, I will ask you about your cycles and whether there is a noticeable relationship between your period and your acne breakouts.
I will need to examine the areas affected by acne closely. Sometimes rashes and other skin conditions mimic acne, and what you think is acne may not actually be acne at all. I will look closely at your skin and ask you to tell me what skin care regimen you are using and what skin care products and beauty aids you use that may be contributing to your acne.
Treatment options
Once we determine that your skin problem is indeed acne, we can talk about treatment options. There are several options available:
- antibiotics– oral and topical antibiotics can kill the bacteria that invade clogged pores. The most frequently prescribed antibiotics are minocycline, doxycycline, tetracycline, erythromycin and clindamycin. All antibiotics can have adverse side effects and some should not be used during pregnancy. We can discuss the pros and cons of antibiotic therapy and decide whether oral antibiotics are right for you.
- oral contraceptives– some women have acne that flares in relation to female hormones that influence sebum production in the skin. Some women benefit greatly from birth control pills, but it may take time before you notice a difference in your skin. Birth control pills are not right for all women, so we can discuss your risk profile before deciding whether oral contraceptives might be helpful for you in controlling your acne.
- spironolactone (aldactone)– this drug is actually a diuretic used to rid the body of excess fluid and control high blood pressure. This medication controls fluctuations in the body of the male hormone testosterone and can be useful for women who suffer from hormonal problems who also have acne. It may be used in combination with oral contraceptives. If you take spironolactone, you will need to have your blood pressure checked regularly, as well as have an occasional blood test to check levels of potassium in your blood.
- specialized skin care– I can recommend a skin care regimen based on your skin type to help in controlling your acne. I can teach you about what to look for on labels when choosing skin care products so that you are not throwing your money away on products that won’t do much for you except empty your wallet.
If you suffer from acne that is ruining your self-esteem, make an appointment to come in and see me. With treatment, acne can be controlled successfully.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.
“If you are experiencing back pain, you are in good company. Back pain is one of the most common reasons that people visit their doctor. Back pain may be acute or chronic and is treated in a variety of ways, depending on the cause of the back pain. Back pain can affect your ability to work and your ability to enjoy life, particularly if it becomes chronic. If you injure your back or suffer from chronic back pain, come in and see me so that we can assess the problem and determine how best to treat your pain”.
-Dr. Anatoly Pisman, MD
What is back pain?
Back pain can affect virtually any area of the back, including the neck, the upper back, the mid-back, the lower back or the tailbone area (the sacrum). It is caused by a problem with the bones or joints of the spine, the nerves that lead away from the spine to the rest of the body, or the muscles and ligaments that support the spine.
Back pain may be dull, burning or sharp and may radiate to other areas, including the the hands, the arms, the buttocks, the groin, the legs and the feet. In addition to pain, you may experience numbness or tingling. You may also experience weakness of the extremities.

What causes back pain?
In most cases, no specific cause can be found for back pain. Back pain may be caused by muscle strain. Other potential causes of back pain include:
- disc herniation– a tiny tear in the outer covering of the intervertebral disc which allows the jelly-like cushion to bulge out
- degenerative disc disease– degeneration (wearing down) of one (or more than one) of the intervertebral discs of the spine
- osteoarthritis– wearing down of the discs of the spine caused by wear and tear associated with the aging process
- spinal stenosis– narrowing of the spinal cord causing compression
- trauma– accident or acute injury affecting the back
- inflammatory disease-such as rheumatoid arthritis or ankylosing spondylitis
- infection
- fracture– osteoporosis, in which the bones become brittle and weak and are prone to fracture, may cause compression fractures of the spine
- cancer (rarely)

How do I know whether to seek care for my back pain?
Most back pain will subside with time and rest. You may still need to see me to rule out a serious cause of your back pain, especially if the pain is severe or does not get better after a few days. There are some absolute red flags that should prompt you to make an appointment to see me urgently. These include:
- bowel/bladder problems (inability to urinate, loss of bladder or bowel control)
- numbness, pins and needles in the genitals, buttocks, inner thigh (what we refer to as the “saddle area”)
- sexual dysfunction (such as sudden impotence with back pain)
- back pain associated with fever, weight loss or night sweats
- history of previous cancer
- progressively or rapidly worsening weakness, pins and needles, or numbness
What can I expect when I come in to see you?
If you come to see me complaining about back pain, I will need to know if you know what caused your pain (for example, back pain occurred at work while you were lifting a heavy object). I will also need to know how long you have had the pain, what remedies you have tried (and if they have worked) and what makes your pain worse.
If you are a new patient, I will need to know about your past medical history, whether you have had any surgeries and whether you are allergic to any medications. I may also ask you about your family history. I will want to know if you have ever had back pain before and what transpired over the course of your previous back pain. Did it get better on its own? Did you require treatment and, if so, what treatment did you receive?
I will then need to examine you. I may ask you to change into a gown, as it will be easier for me to see your back and watch how you move. I will likely ask you to perform different movements and bend in certain ways so that I can try to determine precisely where your pain is located. If necessary, I may order diagnostic testing, but generally this is not necessary if I suspect you have strained your back. Based on my examination and your history, I may suggest:
- antiinflammatory medications to reduce pain and swelling
- ice or heat to relieve pain and reduce inflammation (ice is best for the first 48 hours; after that, a heating pad or hot pack can be used)
- gentle stretching exercises
- physiotherapy
- massage therapy
- avoidance of certain activities for a period of time
If you need a note for work, I can provide you with one. If I feel that your back problem is something that I cannot manage, I will refer you to other specialists; however, I am a physical medicine and rehabilitation physician and can therefore manage most common back pain issues.
If you are suffering with back pain for longer than 3 to 4 days that is not relieved with home remedies, make an appointment to see me in the clinic so that I can rule out any serious causes of your back pain.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Cough is one of the most common reasons why people come to see me. Most coughs are not serious and are caused by a virus, but some coughs may be be caused by a bacteria and may require an antibiotic. It can be difficult for people to determine whether a cough is serious or not- this is where I come in. If your cough lingers for a long time after a cold, is accompanied by a fever or shortness of breath, you need to make an appointment to come in and see me in the clinic”.
-Dr. Zimilevich, MD
What is a cough?
A cough is a reflex, the purpose of which is to keep your lungs and airways clear. Coughs can be annoying if they are frequent or they keep you awake at night, but they are important to your body’s defense. In fact, people with weak coughs due to certain musculoskeletal problems often suffer from frequent pneumonia infections because they lack this simple ability to keep their airways clear of germs.
Acute versus chronic cough
Coughs may be acute, caused by a viral or bacterial illness such as the common cold or pneumonia and lasting a week or two, or chronic as in asthma and COPD. Chronic coughs lasting more than a couple of weeks may be caused by:
- allergies
- smoking
- COPD (chronic obstructive pulmonary disease)
- asthma
- medications (i.e., certain blood pressure medications)
- throat problems
- GERD (gastroesophageal reflux disease, or acid reflux)
- CHF (congestive heart failure)
- malignancy of the respiratory tract (i.e., lung cancer)
When should I be concerned about my cough?
Coughs associated with colds will most often go away on their own in a week or two. Sometimes the cough will linger for a short time after the cold symptoms have disappeared. Although the cough may be bothersome, it usually does not require any treatment. Using a cool mist humidifier, drinking plenty of water and/or sucking on cough drops or lozenges may soothe a lingering cough. Sometimes coughs are caused by post-nasal drip (nasal secretions traveling down the back of the throat).
There are certain instances when your cough should prompt you to come see me in the clinic. You should make an appointment if:
- your cough changes in character (becomes deeper, more frequent or produces more sputum than previously)
- you have fever asociated with your cough for more than a day or two
- you have chest pain when you cough
- you have blood in your sputum
- your cough interferes with sleep or other activities
- you have shortness of breath associated with your cough
- your cough lingers long after other symptoms have gone away, or lasts longer than a couple of weeks
- your cough is associated with weight loss, loss of appetite, night sweats or other unusual symptoms
What can I expect when I come to see you about my cough?
When you come in to the clinic to see me regarding your cough, I will first want to know a bit about your past medical history and any medications you are taking if I have not seen you before. I will need to know when the cough started, what other symptoms are associated with it (i.e., sore throat, cold symptoms, fever), whether your cough is productive (you are coughing up phlegm) and what makes your cough better or worse. I will also need to know if you are a smoker.
Once I have gathered some history about your cough I will examine you, which may include:
- looking in your ears, nose and throat
- listening to your chest with a stethoscope for abnormal breath/breathing sounds
- obtaining your vital signs (temperature, blood pressure, pulse, respirations and oxygen saturation)
- feeling your head and neck for enlarged lymph glands
- palpating your abdomen
- listening to your heart
Based on what I find when I examine you, I may order diagnostic tests, which might include a chest x-ray to rule out pneumonia, blood tests to check for hydration status or signs of infection or inflammation, a sputum sample or pulmonary function testing. I may order other tests if warranted.
Once I have all of the information I need, I will base my treatment on what I believe is causing your cough. I will discuss any test results with you and explain any treatments I prescribe. You should feel free to ask me any questions- I will be happy to answer any questions you have.
If you are suffering from a cough that concerns you, make an appointment to come and see me in the clinic. I promise to take your symptoms seriously- that’s the Mill Basin difference.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Respiratory care is a frequent need- after all, millions of people are stricken by respiratory illnesses such as colds and flu every year. Luckily, many of these illnesses are self-limited. Still others suffer from chronic lung conditions such as asthma, emphysema, and other chronic lung conditions. Whether your symptoms are short-lived or require long-term care, I can help. Just make an appointment and come in to see me. Together we can plan how best to treat you”.
-Dr. Bella Zimilevich, MD
What is the respiratory system?
The respiratory system consists of the nasal passages, the larynx (the voice box), the pharynx (the back of the throat below the nasal cavity), the trachea (the windpipe), the bronchi and the lungs. The main job of the respiratory system is to oxygenate our blood, so that blood rich in oxygen can be delivered throughout the body. The respiratory system is also responsible for helping the body to get rid of waste products (CO2), which we breathe out. The diaphragm is a muscle that lies just below our lungs and helps the lungs expand and contract as we inhale and exhale. The actual exchange of oxygen and carbon dioxide takes place in the alveoli, tiny sacs that are located in the lungs.
What are common symptoms associated with respiratory conditions?
Conditions affecting the respiratory system may be obvious, or may be confused for a problem in another body system. The most common symptoms associated with respiratory disease are:
- cough- a common symptom of respiratory illness; may be acute or chronic, depending on the illness
- chest pain– many respiratory illnesses can cause chest pain or discomfort. Chest pain may result from coughing a lot (muscle or rib pain) or from irritation of the pleura, the membranes that cover the lung.
- fever– fever may be caused by inflammation or infection anywhere in the respiratory tract; ir may also occur with mailgnancy (cancer)
- fatigue– fatigue may be due to not having enough oxygen circulating in the blood stream
- hemoptysis– coughing up blood may occur in tuberculosis and in malignancy (lung cancer), but it occasionally occurs from coughing too much, especially in patients taking blood thinners
- wheezing– individuals with asthma may wheeze, this is due to inflammation and swelling in the airways that restrict air movement
- shortness of breath– individuals may feel short of breath if their oxygen levels are low
- malaise– malaise is feeling generally unwell
- sputum production– pneumonia and other infections of the respiratory tract may cause increased sputum production; asthma may also cause this
- headache– headache may be induced by coughing, or it may be related to infection or inflammation
- hoarseness– excessive coughing or infection of the pharynx (pharyngitis) may cause your voice to become hoarse
What respiratory conditions can you treat?
I am an internal medicine physician. I am also a geriatrician. I treat a variety of adult respiratory illnesses, including:
- asthma
- emphysema
- COPD (chronic obstructive pulmonary disease)
- pneumonia
- colds
- influenza
- bronchitis
What can I expect when I come in to see you?
When you come in to see me in the clinic requiring respiratory care, I will need to gather the following information from you:
- past medical history
- allergies (environmental, food and medications)
- family history
I will ask you about when your symptoms started and if they are associated with other signs/symptoms of infection, such as throat pain, rhinitis (runny nose) or fever. I will ask how long you have had your symptoms and what you’ve tried at home to relieve them- what worked and what didn’t help.
Once I have gathered some history, it’s time for me to examine you. I may look in your nose, ears and throat for signs of infection. I will use a stethoscope to listen carefully to your heart and lungs. I may also examine your abdomen for any signs of tenderness. I may also look for any swelling in your legs, as this is sometimes a sign of cardiac disease, symptoms of which can often mimic respiratory disease.
After I have gathered your history and examined you, I will decide if any diagnostic testing is required. This may include a chest x-ray, a sputum sample or blood tests. I may decide to treat you before lab or x-ray results have come back, or I may ask you to return for another visit- this all depends on my findings and what I suspect is causing your symptoms.
If you are experiencing respiratory symptoms (unless you are certain you are suffering from the common cold, which should improve in 7 to 10 days) make an appointment to come in and see me. While some respiratory symptoms are undoubtedly due to a virus or a bacterial infection that may get better on their own without treatment, other symptoms may be due to a more serious respiratory illness requiring care. Call for your appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

If you suffer from elbow pain, chances are you have tennis elbow, or lateral epicondylitis. This condition is often caused by overuse of the arm (repetitive stress) and can be acute or chronic. If you have pain in the elbow, it’s best to get it assessed to rule out other causes of elbow pain. If you do indeed have tennis elbows, there are several treatment options, the most important of which is rest”.
-Dr. Zimilevich, MD
What is tennis elbow?
Tennis elbow is pain that occurs on the outside (lateral aspect) of the elbow, close to where the upper arm and elbow come together. The condition is common in tennis players because of the way tennis players swing their rackets (backhand strokes are usually the culprit), but it can occur in anyone who uses their elbow to excess. Constant twisting of the wrist, (as occurs when using a screwdriver, for example) can cause tennis elbow, so painters, construction workers, cooks and other workers who use their forearm muscles a lot are particularly vulnerable to tennis elbow. Tennis elbow can also occur from a one-time activity such as raking the lawn if it is done to excess. Using a mouse and computer keyboard too much can also give rise to inflammation.
Muscles in your forearm attach to the bone via tendons at the outside of the elbow. Excessive use of your elbow results in tiny tears in these tendons (may be one tendon, or more than one tendon affected). These tiny tears lead to inflammation and irritation and give rise to the symptoms of tennis elbow.
What are the symptoms of tennis elbow?
- pain in the elbow that gets worse gradually (may be worse in the morning upon arising)
- inability to grasp objects due to a weak grasp
- pain radiates from the elbow to the forearm, and even the hand, when an object is grasped or turned/twisted
- redness/swelling over the lateral epicondyle (bony protrusion on the outside of the elbow)
- increasing pain when the wrist is flexed with the arm in a straight position
- point tenderness over the area of inflammation

How is tennis elbow diagnosed?
If you come to see me complaining of elbow pain, I will ask you when your symptoms started and what caused them (if you can remember). I will ask what makes the pain better or worse and what you have tried at home to alleviate the pain. I will examine your elbow for redness, swelling and pain on palpation over the outer aspect of your elbow. I will have you perform different maneuvers with your arm to see which movements reproduce the pain.
Tennis elbow can often be diagnosed based on symptoms and examination. If I have any doubt as to what is causing your symptoms, I may order an x-ray of your elbow. The x-ray will rule out other problems, such as a fracture, and will show if you have soft tissue swelling around the elbow joint. You can’t see tendons on an x-ray. X-rays are performed to rule out other concerns, not to diagnose tennis elbow.
Can tennis elbow be treated?
Yes, tennis elbow can be treated. Sometimes it takes a long time, and it requires your cooperation. The most important part of treatment is to rest the elbow. You will need to stop doing whatever activity it was that caused the tennis elbow to occur. If you got tennis elbow from the type of work you do, you may need to take some time off work.
Drugs that reduce inflammation may help with the pain and decrease swelling, so I may prescribe an anti-inflammatory agent, either prescription strength or over-the-counter. You should also ice the area 3 times a day for the first week or so. There are tennis elbow braces that can help to decrease pain when you use your affected arm- these can be purchased in any pharmacy or home health store.
If the above measures don’t help, I can inject a corticosteroid into the elbow, which often relieves symptoms for weeks or even months. We can discuss this option if rest, ice and anti-inflammatories do not help. However, rest is the most important thing you can do to help your tennis elbow heal faster. If you continue to use your elbow, your symptoms may become chronic.
If you have had tennis elbow for longer than 6 months to a year and your symptoms have not improved, it may be time to talk to a surgeon. Surgery does not always help with tennis elbow, but it is an option for some. If you need a referral to a surgeon, I can provide you with one.
If you have tennis elbow, it is important that you make sure that tennis elbow is actually the problem. If you have elbow pain it is best to have your elbow assessed. Make an appointment to see me in the clinic.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.
“The hallmark features of a musculoskeletal issue are pain and disability. If you have neck pain, back pain or hip pain caused by arthritis or another condition, you are likely to have intermittent or constant pain and a reduced ability to perform certain activities. While some musculoskeletal problems are due to aging or injury, others are due to immunological problems, such as rheumatoid arthritis. If you suffer from pain requiring musculoskeletal care, make an appointment to come in and see me. I can help you to manage your pain and return to your usual routine as quickly as possible”.
-Dr. Anatoly Pisman, MD
What is musculoskeletal care?
The musculoskeletal system is made up of bones, muscles, joints, cartilage, tendons and ligaments. All of these components work together to give us the ability to move our bodies in a variety of ways. A problem with any of these structures can result in pain, limited mobility, swelling, redness and other symptoms. Generally pain is the largest feature of any problem involving the musculoskeletal system and will be the symptom that results in you making an appointment with me! Musculoskeletal care is care of any of these structures or parts.
How the musculoskeletal system works
It’s important to understand how the different parts of this system work together before we can understand how certain conditions can affect this system.
- Bones (adults have 206 bones in total) provide support and shape to our bodies, and they also protect vital organs. In addition, bones produce certain blood components and store important minerals, including calcium and phosphorus.
- Muscles are attached to bones and are arranged in opposing groups around our joints, which allows us the freedom of movement in different directions at the joints (unless we have joint disease). Our muscles are controlled by nerves, which are in turn controlled by our nervous system.
- Tendons connect muscles to bones and are composed of tough bands of connective tissue. Tendons are attached to bones ; as we contract our muscles, the tendons transmit this force to the bone and pull on the bone, causing it to move. Tendons are quite stretchy, which allows them to act as a spring during movement, which in turn helps us to save energy. Although tendons are stretchy, they have limits- exceed this limit and the tendon can be damaged.
- Ligaments act as the connection point between bones- they join bones together to form a joint. Ligaments act to prevent bones from moving too far out of alignment (dislocating) or breaking. Made of a dense elastic tissue, they can stretch substantially- again, if they are stretched too far, they can be damaged, resulting in an “unstable” joint, or one that is prone to partial or total dislocation.
- Cartilage is a flexible connective tissue found all over our bodies. Cartilage acts as a shock absorber in our spine between the intervertebral discs and between the bones that make up our joints. Cartilage does not contain blood vessels. Because its blood supply is limited, cartilage cannot regenerate easily. Arthritis is a result of a wearing out of the cartilage, resulting in a loss of cushion between the bones of joints such as the hips and knees.
- Bursa are small fluid-filled sacs that cushion joints and can be found around almost every major joint in our bodies. Sometimes a bursa can become inflamed, causing a condition known as bursitis, which cause pain, swelling and limited movement of the affected joint.
What conditions affecting the musculoskeletal system can you treat?
I am a physical medicine and rehabilitation physician. I am able to manage a large number of musculoskeletal conditions, including:
- low back pain
- neck pain
- tendonitis
- bursitis
- arthritis
- gout
- fibromyalgia
- hip and knee pain
- sprains and strains
What Can I expect when I come to see you?
If you come to see me in the clinic requiring musculoskeletal care, chances are you are experiencing one or more of the following symptoms:
- pain
- redness
- swelling
- decreased range of motion
- numbness or tingling
- muscle weakness
- stiffness
- loss of function
First of all, I will want you to tell me about your symptoms, including when they began, what makes them worse or better, what precipitated your symptoms (if you know), what you have tried and whether any self-help measures helped at all. I will also ask about your medical history, your family history, what medications you are taking (including herbal and over-the-counter remedies) and whether you have any allergies.
Once I have a good understanding of your health status and what brought you to see me, I will examine the affected area. I may ask you to change into a gown to allow me to better visualize the affected area, and to allow you to move freely without restriction. I may perform various maneuvers to try to duplicate the pain you are experiencing- do let me know if the pain is severe! I will explain what I am doing and why I am doing it as I go along. I will be looking for reduced movement/stiffness, pain, redness, swelling and other signs and symptoms that may provide clues as to what the problem is.
Once I have examined you and gathered your history, I might order diagnostic tests, such as blood work, x-rays or other tests. If I decide to order any tests, I will tell you what the test is looking for and why I feel it is necessary. Once your test results are available, I will discuss the findings with you. I may prescribe rest, medications such as pain relievers or anti-inflammatories, or other treatments. Again, I will explain any treatments to you and what I hope we can accomplish with treatment. I may also request that you come in again for follow-up. If I think you may have a problem that is beyond the scope of my practice, I will refer you to a specialist.
If you are suffering from musculoskeletal pain or disability, make an appointment to come in and see me. I will ensure you get the right diagnosis and the right treatment.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Even minor burns can be quite painful. Although most minor burns can be managed at home, a large second degree burn often needs medical attention. Third degree burns should be seen in the emergency room, but all other burns can be managed here in the clinic. If you have suffered a burn and are experiencing pain, or the burn is deep and has blistered, make an appointment to have your burn evaluated.”
-Dr. Zimilevich, MD
The Skin
In order to discuss burns, it’s helpful to have an understanding of how the skin is layered. This makes it easier to understand how burns are classified.
The top layer of the skin is called the epidermis. It consists of three layers and contains melanocytes, which are the cells that produce skin pigment (melanin). Just under the epidermis is the dermis, a thicker layer containing sweat glands, hair follicles, nerves and blood vessels, all held together by collagen. The dermis is what gives our skin its strength and stretchiness. Touch and pain receptors are also found in the dermis. Under the dermis is the subcutaneous layer, or hypodermis, which is formed from a network of fat cells and collagen. It acts as a sort of shock absorber and helps us to stay warm. Under theses layers are the muscles, bones, ligaments, cartilage and joints.
Our skin serves many functions. It acts as a barrier, protecting us from injury, infection and dehydration. It is also a sensory organ- without skin we could not feel. Your skin is your largest organ. It is thickest on the soles of your feet and thinnest on your eyelids.
What is a burn?
A burn is simply an injury to the skin caused by heat (thermal burns), chemicals, electricity, radiation or friction. Burns can be further classified according to source i.e. heat, or thermal burns, may be caused by fire or hot water (scalds). All burns, no matter their source, cause some degree of damage to the skin.
Degrees of burns
You have probably heard of burns described in terms of degrees. Here is what the terms first, second and third degree burn means:
- First degree burns affect only the epidermis. The skin is reddened, dry, painful or tender to touch and may be slightly edemetous (swollen). A sunburn is a good example of a first degree burn. These mild burns generally heal in a week or so.
- Second degree burns affect the epidermis and the dermis. They are sometimes subdivided into superficial second degree burns or deep second degree burns, depending on how much of the dermis is damaged. Obviously, the deeper the burn the greater the severity. Second degree burns are moist or dry (depending on depth) and usually painful because nerves are affected (remember that the dermis houses nerve endings). There will be swelling and blister formation. Second degree burns take longer to heal (anywhere from a few weeks to 2 months) and may cause permanent scarring. Severe second degree burns may require skin grafting.
- Third degree burns involve all the layers of the skin. The skin may appear white and leathery or charred. Pain may be less because nerves are destroyed (but this doesn’t mean there will be no pain because burns are often “mixed” with areas of second and third degree burns in close proximity). These burns are life-threatening because the loss of skin puts the victim at risk of massive fluid loss and infection. Skin grafting is necessary. Amputation may also be necessary. Healing may take many months and there is always scarring.
Burns are also sometimes described as partial-thickness or full-thickness, depending on the depth of the burn and layers affected.

First aid at home
For first degree burns or second degree burns that are no larger than 3 inches in diameter:
- cool the burn- run the affected area under cool running water for several minutes or apply a cloth or towel soaked in cool water to the affected area
- cover the burn with a dry, clean dressing to prevent infection and reduce pain (don’t use any material such as cotton batting that may leave material in the wound)
- use an over-the-counter pain reliever for pain (do not give aspirin to children under 12 years of age)
Do not apply butter or other greasy agents to the burn- this may cause infection. If blisters are present, do not break the blisters- allow them to break on their own. Lastly, do not apply ice to the area as this may further damage the skin.
If you have a second degree burn that is larger than 3 inches in diameter or a third degree burn, you should seek medical attention right away. If someone you know has been burned over a large part of their body call an ambulance so that they can be transported to the nearest emergency room.
What can I expect if I need to come in because I have burned myself?
If you have burned yourself, you need to come in as soon as possible after being injured. I will ask about your medical history, any medications you are taking and whether you are allergic to any medications. You will need to tell me how you were burned and how long it has been since the injury occurred. I will examine the burned area to determine the severity of the burn. Depending on the extent of the burn, I may prescribe an antibiotic ointment or oral antibiotic if I am concerned about infection. You may need daily dressing changes- if this is the case, I will instruct you on how to perform the dressing change or make arrangements for daily dressing changes. In some cases, you may also need a tetanus shot if you have not had one for a while. If necessary, I may refer you to a specialist (plastic surgeon).
If you have suffered a burn, call to make an appointment as soon as possible. In most cases, we can see you very quickly. Doing so may prevent infection and other complications.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Osteoporosis causes bones to become weak and brittle, making them more prone to fracture. Osteoporosis is a serious disease that can result in serious disability. As you get older, your bones also age, losing mass, especially in women after menopause. Osteoporosis can be halted, and sometimes prevented, by diet and exercise. If you have been told that your bones are weak, we can work together to prevent disease progression and protect you from breaking bones”.
Dr. Bella Zimilevich, MD
What is osteoporosis?
Osteoporosis is a disease of the bones. It is characterized by low bone mass. Bone tissue deteriorates over a long period of time, resulting in bones that are brittle and weak. Because the bones are brittle and weak, they can break easily. Osteoporosis rarely causes symptoms until the disease is well under way, earning it the nickname of “the silent thief”, because it steals bone mass without you knowing it. The spine, hip, wrist and shoulder are the bones that break most commonly in osteoporosis.

What causes osteoporosis?
There is no one single cause of osteoporosis. It can strike men and women of any age, although the condition is more common among older patients. Risk factors for osteoporosis include:
- age– osteoporosis is more common in older individuals
- sex– osteoporosis is more common in women
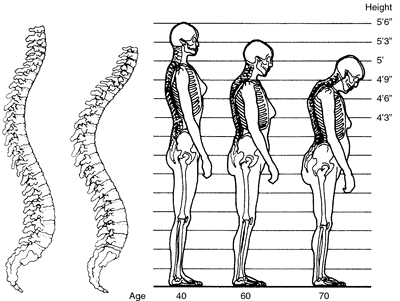
- menopause– all of us begin to lose bone in our 30s; after menopause, women lose bone at an accelerated rate (up to 2 to 3% per year)
- glucocorticoid drugs– steroid use for longer than 3 months increases the risk of osteoporosis
- malabsorption– medical conditions that inhibit the absorption of nutrients such as calcium and vitamin D can lead to osteoporosis
- medical conditions/medications- these may contribute to, or speed up, bone loss (i.e. thyroid disease, parathyroid or adrenal gland disorders)
- race– Caucasian and Asian women are more prone to developing osteoporosis
- size– individuals who start out with a small frame are more likely to develop osteoporosis (i.e., someone who is 110 pounds with a tiny frame may be at higher risk than someone who is 200 pounds with a large frame)
- lifestyle– a sedentary lifestyle, drinking too much alcohol, cigarette smoking and poor diet may all contribute to the development of osteoporosis
If you parents suffered a hip fracture or a compression fracture of the vertebra, you may be at higher risk for osteoporosis. Loss of height may be an indication of osteoporosis.
What are the symptoms of osteoporosis?
As mentioned, there are often no symptoms of osteoporosis until a fracture occurs. If your osteoporosis is fairly advanced you may experience:
- loss of height over time/stooped posture
- back pain
- bone fracture that occurs after an inconsequential event, such as bending over or sneezing, or a fall that normally would not cause a bone to break
How is osteoporosis diagnosed?
Bone densitometry is a special type of x-ray that can measure the density of bones. Usually only a few bones are checked, such as your wrist, spine and hip. With this test, the density of your bones is compared to others of the same height, weight and age. Sometimes regular x-rays will raise the suspicion that your bones are thinning, which may prompt me to order a bone density test.
What can I expect when I come in for my appointment?
When you come in to see me and you are concerned about osteoporosis, I will start by asking about your past medical history and that of your family, as a family history of osteoporosis is important. I’ll ask you about medications you are taking or have taken in the past (such as steroids) that may have a bearing on the condition. I’ll ask about diet and lifestyle factors that may be of concern. I’ll measure your height to see if it has changed or remained stable. If you are a woman, I’ll determine if you are premenopausal or postmenopausal, as this may put you at higher risk. If you have back pain or have already suffered a fracture, I may want to see old x-rays, and I may order new x-rays for comparison. I will order a bone density test if needed.
We can discuss your personal risk factors for osteoporosis and what you can do to decrease your risk of developing osteoporosis, or prevent it from getting worse and protect you from fractures if you already have it. Exercise, diet, supplementation with calcium and vitamin D, quitting smoking and reducing alcohol intake can all help to arrest the disease. There are medications that can be prescribed if you have osteoporosis to help slow bone loss.
If you have or suspect you may have osteoporosis, you should come in and see me as soon as possible. The sooner we reduce your risk factors, the sooner we can stop the process of bone loss and protect you from suffering a fracture.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“With the temperatures outside extremely hot and with humidity soaring, you should know how to protect yourself against heat exhaustion. Heat exhaustion can lead to heat stroke, which can be life-threatening, particularly for people who are elderly or those who have heart and lung conditions. If you think you, or someone you know, has heat stroke it’s important to get out of the heat and seek immediate care”.
-Dr. Zimilevich, MD
About Heat Exhaustion/Heat Stroke
Simply put, heat exhaustion occurs when your body becomes overheated. Normally, your body cools itself by sweating. Body temperature is controlled by a part of your brain known as the hypothalamus, which maintains the body’s temperature within a fairly narrow range. When you are outside in very hot weather and don’t replace the fluids your body loses through sweating, the hypothalamus is overwhelmed and begins to produce more heat than the body can handle by sweating. Heat exhaustion is a form of dehydration caused by exposure to excessive heat for prolonged periods, or from drinking fluids that don’t contain enough sodium (salt).
Heat stroke is a more serious form of heat exhaustion and can lead to coma and even death if not treated. People with heat stroke may be confused with dry skin. Heat stroke occurs when heat exhaustion is not treated.
Symptoms of Heat Stroke/Heat Exhaustion
If you have heat exhaustion, you may experience:
- dizziness/weakness/fainting
- rapid heart rate (tachycardia)
- thirst
- excessive sweating
- nausea vomiting
- muscle cramping (heat cramps)
- pale, cool and clammy skin
- fatigue
- headache
- elevation in temperature (most often a mild rise)
In heat stroke, the body temperature exceeds 40 degrees Celsius (104 degrees Fahrenheit) and coma or seizure may follow. Heart attack and death may also occur. Heat stroke is an extremely serious condition.
Who is Most at Risk?
Certain people may be at higher risk of suffering from heat exhaustion. If you fall into one of the following groups, you should be especially cautious when outdoors in hot weather:
- you are already dehydrated (i.e., have had vomiting or diarrhea, or have been unable to drink enough fluids)
- you are drinking beverages containing alcohol
- you are elderly
- you have chronic respiratory disease
- you are obese or overweight
- you have hypertension (high blood pressure)
- you are pregnant
- you have chronic heart disease
- you are working outdoors performing physical labor
- you are taking medications that may interfere with your body’s ability to cool itself (i.e., beta-blockers, tranquilizers, antihistamines)

How to Prevent Heat Stroke
- The best offense is a good defense- try to avoid the sun during the hottest part of the day whenever possible. If you must be outdoors:
- drink more fluids than normal, and ensure that you are not drinking fluids that don’t contain any sodium at all
- check on elderly friends and neighbors and those who may be vulnerable to the heat regularly to ensure they are staying cool and are not victims of the heat
- avoid drinking alcohol if you must be out in the sun
- if you must do chores outdoors, wait until it is cooler out before venturing outdoors (i.e., early morning or evening hours)
- dress appropriately in cool clothing
- if exercising outdoors, drink 2 glasses of water prior to exercising and a glass of water every 20 to 30 minutes thereafter
- take cool baths if you are feeling overheated
- use fans indoors if you don’t have air conditioning
- remember never to leave anyone who is vulnerable (babies, the elderly, small children or disabled individuals) in vehicles in the heat
What to do if you think you have heat exhaustion:
If you think you, or someone else, may have heat exhaustion, get to a cool place out of the heat. Remove any excessive clothing. You can place ice packs on the back of the neck and head and in the armpits and groins-this will cool the body quickly. You can also use fans or a cool bath to lower body temperature (do not put someone who is not fully conscious in the tub and leave them unattended). Replenish fluid loss by drinking water, naturally sweetened fruit juices or sports drinks.
If you or the person you are treating do not feel better after 20 minutes, you should be seen by a medical professional. If the person is semi-conscious or fully unconscious call an ambulance for immediate assistance.
If you come to see me in the clinic with symptoms of heat exhaustion, I will assess your temperature, pulse, respirations and blood pressure. I will examine you for signs and symptoms of dehydration. I may order diagnostic tests such as blood work or a urine test to assess the extent of dehydration. I may also use cooling measures to bring your body temperature down.
The best way to avoid heat exhaustion and heat stroke is to avoid the heat as much as possible. If you or someone you know are experiencing symptoms of heat exhaustion, call for an immediate appointment.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.
 “Constipation is an embarrassing topic for many people, although it is very common. It can cause abdominal discomfort, nausea and loss of appetite. If left untreated, severe constipation can lead to mechanical obstruction. If you suffer from frequent or chronic constipation, you want to be sure that there is not an underlying problem causing your constipation. Make an appointment to see me so that I can help you get your bowels back on the right track”. Dr. Zimilevich, MD
“Constipation is an embarrassing topic for many people, although it is very common. It can cause abdominal discomfort, nausea and loss of appetite. If left untreated, severe constipation can lead to mechanical obstruction. If you suffer from frequent or chronic constipation, you want to be sure that there is not an underlying problem causing your constipation. Make an appointment to see me so that I can help you get your bowels back on the right track”. Dr. Zimilevich, MD
Constipation defined The definition of constipation varies from person to person. While some people may have a bowel movement every single day, others may go 2 or 3 days between bowel movements and feel just fine. Therefore, constipation can be defined as less than 3 stools (bowel movements) per week and/or difficulty passing stools. If you are going every day or two but have to strain to pass very hard stools, you are constipated!
What causes constipation? The list of conditions that can cause constipation is long. The following are some of the more common causes:
- dehydration/not drinking enough fluids- when your body is low on fluids, your intestines will draw more fluid from stools (or add less water to stools), making them harder to pass
- not enough fiber in your diet- many of us fail to eat enough fiber in our diets (women should consume about 21 to 25 grams of fiber; men should consume about 35 to 38 grams of fiber per day)
- sedentary lifestyle- older people and people who do not get enough exercise are more likely to become constipated
- medications- many medications can cause constipation, including narcotic pain medications, certain blood pressure medications, antidepressants and others
- ignoring the urge to “go”/delaying the urge- sometimes we ignore the urge to have a bowel movement because it isn’t convenient (i.e., you’re too busy at work to stop what you are doing); ignoring the urge may lead to constipation
- changes in routine/lifestyle- pregnancy, aging, travel and other changes in your regular routine can lead to constipation
- laxative abuse- ironically, using laxatives too often can lead to a lazy bowel that won’t work well without more laxatives, thus creating a viscious cycle that can be difficult to break
- specific medical conditions- stroke, diabetes, Multiple Sclerosis, Parkinson’s disease and other health conditions can affect bowel movements
- bowel problems- diverticulosis, bowel obstruction and other bowel conditions may have constipation as one of the major symptoms
- IBS- IBS is a functional bowel disorder that results in diarrhea, constipation or a combination of the two; IBS is a functional bowel disorder which is very common
- hormonal disturbance- thyroid gland dysfunction and other disorders of the glands may cause constipation
- spinal cord injury- many spinal cord injury patients suffer from constipation due to damage to nerves that innervate the bowel
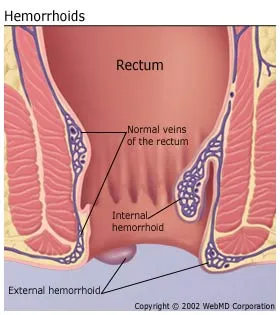
- hemorrhoids/anal fissures- painful rectal or anal conditions may cause constipation because these conditions are painful, and sufferers may be reluctant to have a bowel movement due to pain; in addition, anal sphincter muscles may spasm, making it difficult to have a bowel movement
 What symptoms can be caused by constipation? As we discussed, passing fewer than 3 stools per week or passing hard stools/straining at stools are part and parcel of constipation. If you are constipated, you might also experience:
What symptoms can be caused by constipation? As we discussed, passing fewer than 3 stools per week or passing hard stools/straining at stools are part and parcel of constipation. If you are constipated, you might also experience:
- a sensation of stool in the rectum/rectal blockage
- a sense of incomplete evacuation
- bloating/cramping/abdominal discomfort
- mild nausea
These symptoms are common in constipation. If you are frequently constipated, you should make an appointment to see me in the clinic. What symptoms might signal a more serious problem? If you are constipated and experience any of the following symptoms, you should come in as soon as possible to be assessed:
- blood in your stool
- weight loss
- fever
- vomiting
- inability to pass flatus (gas)
- severe abdominal pain
- increasing abdominal girth (your abdomen seems to be growing steadily and you’re not pregnant)
- thin, ribbon-like stools
- pain in the rectum
These symptoms may signal a more serious problem, such as rectal or bowel cancer, inflammatory bowel disease or an infectious process.
What can I expect at my appointment? When you come to see me complaining of constipation, I’ll ask about your bowel habits. I will want to know how often you have a bowel movement, whether your stools are hard and whether you have to strain to pass stools. I’ll want to know if you have any medical problems that may be causing constipation. Please bring all of your medications (or a list of your medications) if I am seeing you for the first time so that I can rule out any medications as being to blame. I will also want to know how often you exercise and how may cups of water/how much fluid you drink in a day. I’ll want you to tell me about your typical diet so that we can determine whether lack of fiber may be contributing to the problem. You can estimate the number of servings of fruits, vegetables and grains you eat in a day. Better yet, keep a food diary for a week prior to your visit- this can really be helpful to me to help me pinpoint how you can improve your diet. I may want to examine your abdomen so that I can see if any areas are tender or any masses are present. Blood work, abdominal x-rays and other tests may rule out any serious problems, allowing me to focus on lifestyle remedies and possibly medications to treat your constipation. 
Home remedies for constipation If you suffer from constipation, there are several things you can do to try to regulate your bowels:
- increase the amount of water/fluids you are drinking
- avoid caffeine and caffeinated beverages, as these may worsen constipation (caffeine is a mild diuretic)
- try drinking a cup of warm water first thing in the morning (you can flavor with lemon if desired)
- do not ignore the urge to have a bowel movement
- increase your activity- walking is an excellent bowel stimulant
- increase the amount of fiber you are eating
If none of the above remedies help you achieve more regular bowel habits and you are still constipated, make an appointment to come in and see me in the clinic. Together, we’ll get to the “bottom” of your constipation.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“An ear infection can be extremely painful. If left untreated, otitis media can lead to permanent hearing loss. If you have a severe ear ache, particularly if you have been sick with a cold or other viral infection, make an appointment to come in and see me right away”.
-Dr. Zimilevich, MD
What is otitis media?
Otitis media is the medical term for infection of the middle ear. This condition is far more common in children than in adults but can cause considerable pain regardless of age.
What causes otitis media?
Acute otitis media often occurs after a cold or other illness and can be caused by a virus or bacteria. It is more common during the winter months when colds are more prevalent.
What are the symptoms of otitis media?
If you have otitis media, you may notice:
- ear pain (may be severe)
- hearing loss in the affected ear
- fever
- nasal congestion or sore throat if otitis media is preceded by a cold
- bloody discharge from the ear if the tympanic membrane (eardrum) ruptures (pain may disappear if this happens)
What can I expect when I come in for my appointment?
If you have otitis media, you may need to be seen urgently. The pain can be quite severe and overwhelming. I’ll ask you about your symptoms- when they started, whether they were preceded by a cold and whether you have had a fever. I’ll look in your nose and throat for signs of infection/inflammation. I may also listen your chest if you have had a cough. I’ll use an otoscope (an instrument with a light attached) to examine your ear, looking for fluid, redness, pus and bulging of the tympanic membrane. If you have otitis media, I’ll need to know if you have any allergies to any medications, especially antibiotics.
What is the treatment for otitis media?
If you have otitis media, you will (quite understandably) be concerned about the pain and how long it will last. Although acetaminophen (Tylenol) or ibuprofen (Motrin) may help with the pain and fever, you may need something stronger for the first couple of days. I will also prescribe an antibiotic if I suspect a bacterial cause. If you are prescribed an antibiotic, it is important that you take it exactly as prescribed; otherwise, the infection may return and be more difficult to treat. Always complete the entire course of antibiotics! Sometimes an antihistamine or decongestant medication can be helpful in reducing congestion and may improve the sensation of pressure and fullness in the ear that some people feel when they have an ear infection. If you are still experiencing symptoms (including hearing loss) after you have completed antibiotics, you should come back to see me for follow-up.
If you are experiencing ear pain, make an appointment immediately- in most cases we can see you right away, so make your appointment now.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Eczema is not only itchy and uncomfortable, but can lead to bacterial skin infections when affected areas are scratched. There are a number of treatment options available. If you suffer from eczema you should be examined, first to ensure that eczema is actually the problem and second to find a treatment that works for you”.
Dr. Bella Zimilevich, MD
What is eczema?
Eczema is a very common skin condition, estimated to affect 1 in 5 people in their lifetime. There are numerous types of eczema, with atopic dermatitis being the most common. Atopic dermatitis often begins in childhood, although it can develop later in life. People with atopic dermatitis often have a genetic tendency to the condition. Eczema, hay fever and asthma are all closely linked and can be seen running through families.
In atopic eczema, the skin is very dry and itchy. Eczema can be influenced by environmental factors, such as weather, contact irritants and temperature. The skin if often very sensitive to chemicals found in soaps, cleaners and detergents. In acute flares of eczema the skin is red, inflamed, and sometimes blistered and weeping. In adults, eczema most often affects the hands, eyelids, elbow creases and knee creases, but it can occur anywhere on the body.
Certain occupations may give rise to a worsening of eczema, due to the fact that the hands are often in contact with chemicals and other irritants. Housekeeping, hairdressing, caregiving, farming and industrial cleaning are all occupations in which high numbers of workers have eczema.
What causes eczema?
No one knows for certain what causes eczema, but there are many theories:
- atopy- atopy is the genetic tendency to hay fever, asthma and eczema. Atopy is inherited and involves an exaggerated immune response to environmental triggers.
- skin barrier defect- may experts believe that people with atopic dermatitis have a defect in their skin which allows moisture to leave the skin, rather than be kept within it. There may also be reduced antimicrobial function, or a decreased ability of the skin to fight infection.
- altered immunity- the specialized immune cells of the skin have an increased response to antigens, resulting in inflammation
It’s likely that all three of these theories are correct to some degree and all work in concert in individuals with contact dermatitis.
What are the symptoms of eczema?
- red patches of skin (may also be reddish-brown or gray over time)
- itchiness (may be worse at night)
- thickened, scaly or cracked skin
- small raised bumps on the skin (may leak fluid and form a crust when scrathched)
- raw, painful skin due to scratching

Many people with atopic dermatitis also develop bacterial infection of the affected areas caused by Staphylococcus aureus, which is commonly found on the skin and can invade eczematous patches of skin through scratching. Bacterial infection may worsen symptoms.

Treatment for eczema
Treatment for eczema generally involves several components. The most important is to moisturize the skin using emollient lotions or creams. Topical corticosteroids may be used to reduce inflammation; however, they should not be used for long periods of time as they can have adverse effects, including thinning of the skin over time. Antihistamines can be used to reduce itching. These medications cause drowsiness and are most often used at night to promote sleep when itching is severe. Medications that decrease the immune response may also be used for some people with contact dermatitis. When infection is present, a topical or oral antibiotic may be prescribed.
If you have eczema, you should avoid:
- excessive bathing, especially when bath water is very warm
- use of heavily perfumed soaps and lotions
- scratching the affected areas (some people wear cotton gloves at night to prevent scratching)
- clothes that don’t allow your skin to breathe, such as spandex and nylon-based wear
- contact with known triggers, such as harsh cleaners or detergents
What can I expect when I come in for my appointment?
When you come in to see me, I will ask about your medical history, as well as your family history. I’ll want to know if any family members have eczema, asthma or hay fever. I’ll also want to know if you have any known allergies. I will ask about your symptoms, when they started and what you have used on your skin. I’ll also ask about possible triggers and your occupation to try to identify anything that might make your eczema worse. I’ll examine the affected area(s) to determine how severe your eczema is and look for signs of infection.
Once I have finished my examination, we’ll come up with a treatment plan together. I may prescribe a corticosteroid cream or an antibiotic if necessary. We can discuss any lifestyle factors or environmental factors that may be causing or worsening your eczema.
If you have eczema it is best not to ignore it, especially if it your skin is acutely reddened and inflamed. With the right treatment, your symptoms can improve. Make an appointment to see me today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Menopause is called ‘the change’ for good reason. While some women breeze through menopause without any problems, some women experience all of the menopause symptoms- hot flashes, depression, interrupted sleep, weight gain…Menopause is a great time to take stock of your health with a view to thwarting any conditions that may be a problem in the future. If you think you are in menopause, whether you are just starting the process or are nearing the end, come in and see me so that we can discuss what changes you can expect and plan for your healthy future”.
-Dr. Zimilevich, MD
What is menopause?
Medically speaking, a woman is said to be in menopause when she has not has a period for one full year. At this point, ovulation no longer occurs and a women can no longer become pregnant. Perimenopause is the period before menopause when estrogen levels begin to decline. Perimenopause can last several years. When women talk about menopause symptoms, they may be in the perimenopause period or may already be menopausal. It is the absence of the menstrual period for a period of one year that defines menopause. Women may have very irregular periods leading up to menopause.
What are the symptoms of menopause?
Symptoms of menopause can affect virtually every system of the body and can vary between women. No woman will experience menopause in exactly the same way as another. If you are nearing menopause you may experience:
- irregular menstrual periods– periods may be very irregular and you may even skip several months between periods; they may also be heavier or lighter than normal
- infertility– older women (women in their 40s) may have difficulty becoming pregnant as estrogen levels drop
- vaginal discomfort and dryness- as estrogen levels decline, natural lubrication of the vagina also diminishes, which may result in vaginal dryness. Some women experience discomfort during intercourse. Vaginal atrophy refers to thinning and shrinking of the vaginal tissues, which can cause inflammation.
- hot flashes– hot flashes are the most notorious of all menopause symptoms. Hot flashes involves a sensation of heat in the head, face and chest. These sensations occur suddenly and without warning and may be accompanied by palpitations or a racing heart. Hot flashes may last for a few seconds to a minute or more. They may leave you feeling weak and clammy.
- night sweats– if you wake up drenched in sweat even when the room is cool, you may have had a night sweat. These are similar to hot flashes but occur at night, often interrupting sleep
- disturbed sleeping patterns– night sweats may keep you awake, but you may also be kept awake by anxiety or have difficulty falling asleep or staying asleep
- mood swings– irritability is common in menopause and may be due to lack of sleep if sleep is interrupted. Rapid mood swings may also occur in women who are not sleep deprived. You may find yourself see-sawing between tears, laughter and every emotion in between
- urinary issues– lack of estrogen can contribute to weakened pelvic floor muscles, resulting in incontinence. Urinary tract infections are more common. Urinary frequency may occur.
- joint pain– some women experience more frequent joint pain, or a worsening of preexisting joint pain.
- headaches– some women experience more frequent headaches, while other women find that their headaches improve.
- cognitive difficulties– difficulty in remembering and processing information may occur; forgetfulness is a frequent complaint
- weight gain– muscle is replaced by fat, especially around the abdomen, and you may find it harder to lose weight
- breast changes– breasts may atrophy (become smaller) due to lack of estrogen, and nipples may become smaller and flatter than before
- hair changes– scalp hair may thin and become weaker and more brittle
- bones– bones lose mass and become weaker in some women, leading to osteoporosis
- skin changes– the skin becomes drier and less elastic after menopause
- depression– some women experience depression before, during or after menopause. This is often due to fluctuating hormones and may be transient

How is menopause diagnosed?
If you have not had a period in a year or longer, it is safe to say you are in menopause! Otherwise, there is no sure way to diagnose menopause. Measuring FSH (follicle stimulating hormone) levels can give us an idea that you may be approaching menopause because FSH levels tend to rise as estrogen levels decrease; however, this is a far from perfect science as FSH levels can fluctuate wildly. The symptoms you are experiencing will provide many clues- if you have many of the symptoms you are likely approaching menopause.
What can I expect when I come to see you?
When you come in to see me and you suspect you may be in menopause, I’ll start by asking you about your periods: How often are you having periods? If your periods have stopped, when did they stop? I’ll ask you about any menopause symptoms you are experiencing and whether they are particularly bothersome. Most symptoms will pass with time; if they are impacting on your life, we can talk about how to manage them.
We’ll also discuss your risk factors for certain conditions, such as osteoporosis and heart disease. Menopause can raise your risk for certain health problems, so from now on it will be important that I see you regularly for checkups.
Menopause is the ending of one phase or your life and the beginning of another. Many women are glad to say goodbye to their periods, while others feel sad that their childbearing years are over, even if they did not plan on adding to their family. If you are feeling conflicted, this is perfectly normal. If you feel blue for a while that’s okay too- but if you feel depressed for longer than a few weeks and your symptoms are not improving, it’s time to do something about them.
If you are experiencing symptoms of menopause, come in and talk to me. Together we can determine where you are in your menopause journey and discuss ways to manage menopause symptoms. Make your appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“As you age, your prostate will start to enlarge and may eventually cause problems. This generally begins to happen after age 40 and is very common. An enlarged prostate can eventually begin to put pressure on the urethra, causing difficulty with urination. While an enlarged prostate does not mean you have cancer, you should be seen for regular physical exams. If you are experiencing difficulties with urination, help is available. Many men are uncomfortable discussing their prostate and any issues it may be causing. You shouldn’t feel embarrassed- most men experience this issue at some point as they get older.
-Dr. Zimilevich, MD
What is the prostate and what does it do?
Your prostate gland is walnut-shaped. It sits at the base of your bladder just in front of the rectum. It surrounds the urethra, which is the tube that carries urine from the bladder to the outside of your body. It is made up of two lobes which are encased in a layer of tissue.
The prostate goes through two growth spurts, during puberty and again around age 25. Thereafter, it continues to grow at a slower rate. Approximately half of all men in their 60s and almost all men in their 70s and 80s have symptoms associated with an enlarged prostate.

What symptoms are caused by an enlarged prostate?
The symptoms of prostate enlargement are due to the pressure that the enlarged prostate places on the urethra. This results in urinary symptoms including:
- a weak, hesitant or dribbling urine stream
- urinary frequency (often worse at night)
- urinary urgency
- leaking or dribbling of urine
- inability to empty the bladder
In some cases, these symptoms do not present first; instead, you may suddenly find yourself unable to void (urinate) at all. This is called acute urinary retention and is an emergency.
What are the possible complications of prostate enlargement?
Some men will experience mild symptoms with an enlarged prostate, while others may experience more severe symptoms. A very enlarged prostate may cause urinary tract infection, bladder stones, damage to the bladder and kidneys due to urine backing up in the urinary tract and urinary incontinence (the involuntary leakage of urine).
What can I expect when I come in for an exam?
Whether or not you are experiencing symptoms related to an enlarged prostate, you should be coming in for a prostate exam every year after age 40. The prostate exam is often done as part of a yearly physical. In order to judge the size and contours of the prostate gland, a digital rectal exam is required.
I may also recommend a PSA (prostate-specific antigen) blood test. PSA is a protein that is made by the cells of the prostate. The PSA level may be elevated if you have cancer of the prostate. It is important to know that not all enlarged prostate glands are enlarged because they are cancerous; however, cancer is a possibility when the prostate is enlarged. It is also important to know that the PSA can be elevated for other reasons besides cancer. For example, an enlarged prostate can cause the PSA to be elevated, as can infection of the prostate gland. Although a PSA can be useful, it is not the only piece of information we use to diagnose prostate cancer.
If I am concerned that you may have prostate cancer, I will likely refer you to a urologist, who is an expert on prostate cancer.
What treatment is available for an enlarged prostate that is causing urinary symptoms?
If your symptoms are mild and not particularly bothersome, I may recommend no treatment other than keeping a close eye on the situation through regular checkups.
If your enlarged prostate is causing urination problems that pose a danger to the health of your urinary tract, or your symptoms are very inconvenient, there are medications that I can prescribe that can improve your symptoms. These medications can help to shrink the prostate, or at least stop it from growing any further. Some medications target urinary symptoms, helping to relax the bladder and improve urine flow.
If medication therapy fails to improve your symptoms, a visit to a urologist may be warranted. I can arrange a referral to a urologist if this occurs.
If you are experiencing symptoms that you think may be due to an enlarged prostate, or are due for a prostate exam, don’t delay because of embarrassment- help is available. All you have to do is make an appointment.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Hemorrhoids are a common problem affecting millions of people. Although they can cause pain, discomfort and bleeding, many people are reluctant to seek medical care due to embarrassment. If you suffer from hemorrhoids, you should know that various treatments are available. If you have rectal pain or bleeding, you should come in to be seen to be certain that your symptoms are actually due to hemorrhoids and not another more serious problem”.
-Dr. Zimilevich, MD
What are hemorrhoids (piles)?
Just as you can get varicose veins from standing on your feet for too long, you can get hemorrhoids from activities that place undue pressure on the veins in the rectum. When veins swell within the rectum, they are called internal hemorrhoids. When the veins around the anal opening swell, they are known as external hemorrhoids. It is possible to have both types of hemorrhoids at the same time.
What causes hemorrhoids?
Piles are most common between the ages of 20 and 50- it is estimated that approximately 40% of people suffer from piles at some point in their life, so if you have them you can consider yourself to be in good company!
Hemorrhoids can be caused by:
- weak veins- some people just naturally have weaker veins, which may predispose them to developing both piles and varicose veins
- increased abdominal pressure- pregnancy, obesity, prolonged standing or sitting, frequent coughing or vomiting, and straining during bowel movements are all activities that can increase abdominal pressure and may lead to the formation of hemorrhoids
- diet- people who eat a low fiber diet and/or a lot of processed foods may be at higher risk of developing hemorrhoids; this type of diet can cause constipation, and straining to have a bowel movement can lead to piles
- inadequate fluid intake- not drinking enough fluids can cause stool to become hard and lead to straining during bowel movements; hard stools can also irritate hemorrhoids that are already present, causing them to swell even further or bleed
- chronic diarrhea/constipation- spending a lot of time on the toilet can cause piles
- age- as we age, the tissues supporting the veins in the anus/rectum can become weak
Are there different types of hemorrhoids?
As mentioned, piles may be found internally or externally.
- internal hemorrhoids- these hemorrhoids are located inside the rectum and can’t be seen or felt. They are usually not painful because there aren’t a lot of nerves capable of transmitting pain in the rectum. Bleeding may be your only clue that you have internal hemorrhoids. Sometimes internal hemorrhoids become large enough that they protrude from the anus- these are known as prolapsed hemorrhoids. These can often be gently pushed back inside if they don’t recede on their own. When internal hemorrhoids prolapse they may be painful.
- external hemorrhoids– these hemorrhoids lie just inside the anus and may be felt when you have a bowel movement. Because the anus is innervated with nerves, these hemorrhoids can be painful, particularly if they become thrombosed. A thrombosed hemorrhoid is an external hemorrhoid with a blood clot inside it. If you have a thrombosed hemorrhoid, you will likely be aware of it as these can be very painful. The pain may cause you to seek medical attention.
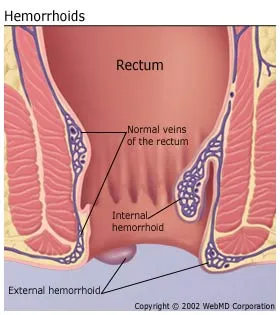
What are the symptoms of hemorrhoids?
If you have hemorrhoids, you may experience:
- bleeding with bowel movements (this bleeding is painless- there may be bright red blood in the toilet bowel or on the toilet tissue)
- discomfort/pain in the rectal area
- swollen areas around the anus
- a painful lump located near the anus
- itching of the anal area
- leakage of small amounts of stool
It can be difficult to judge the amount of blood loss when blood is present in the toilet water. If you experience a change in bowel habits, pass tarry black or maroon stools or the blood is mixed within the stool, you should make an appointment to be seen immediately. Bleeding is most often caused by hemorrhoids, but it can also be caused by colon or rectal cancer or other gastrointestinal diseases. If you feel weak or dizzy and are bleeding from the rectum, you should seek care at the nearest emergency room.
What can I expect when I come in for my appointment?
If you know or suspect that you have hemorrhoids, especially if you are experiencing rectal bleeding, you should make an appointment to come in to see me. I will ask you what symptoms you have noticed, how long you have had the symptoms and what makes your symptoms better or worse. I may ask about your bowel habits (how often your bowels move), whether you have noticed a change in your bowel habits, what you typically eat and how much water or other fluids you normally drink. I will also ask if anyone in your family has ever had bowel or anal cancer. I may decide to examine you. If you have been experiencing a lot of bleeding or have been bleeding for a long time, I may decide to order blood work to ensure that you are not anemic (low in iron/red blood cells) from blood loss.
What is the treatment for hemorrhoids?
Treatment is dependent on whether your hemorrhoids are internal or external and how severe they are. Medicated ointments, creams and suppositories may be helpful to relieve discomfort, swelling and itching. You can also try warm baths for comfort. A high fiber diet and an increase in fluid intake may help to prevent constipation. If your hemorrhoids are severe, I may decide to refer you to a specialist. Surgery is sometimes necessary, but there are also minimally invasive procedures that can be performed to treat hemorrhoids.
If you are experiencing rectal bleeding, it is important to ensure that your bleeding is indeed due to hemorrhoids and not another more sinister condition. It is dangerous to assume that bleeding is due to hemorrhoids without ruling out a more serious problem. If you have hemorrhoids that are causing you discomfort or are experiencing rectal bleeding, make an appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.




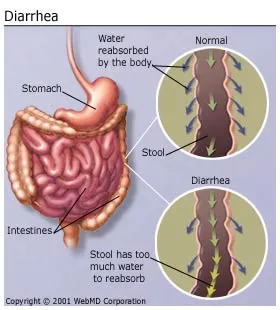







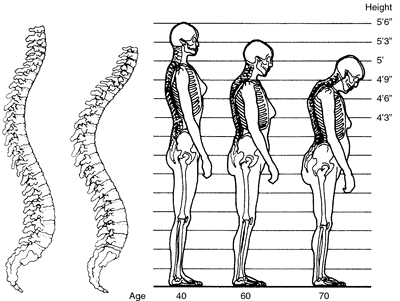

 What symptoms can be caused by constipation? As we discussed, passing fewer than 3 stools per week or passing hard stools/straining at stools are part and parcel of constipation. If you are constipated, you might also experience:
What symptoms can be caused by constipation? As we discussed, passing fewer than 3 stools per week or passing hard stools/straining at stools are part and parcel of constipation. If you are constipated, you might also experience: