Answer: Finding a lump in a breast is enough to strike fear into any woman’s heart. You’re right to be concerned. While many lumps are discovered by women themselves, most are benign- but this doesn’t mean you should ignore them. It takes only a few minutes to check a breast lump, and it is far better to be safe than sorry.
The following are some general rules of thumb. Keep in mind that they are not meant to falsely reassure you (or cause panic):
- Painless lumps are of greater concern than painless lumps
- Hard lumps are of greater concern than soft lumps
- Lumps that are “fixed” in place are of greater concern than lumps that move freely
- Rough, irregular lumps are of greater concern than smooth lumps
- Lumps that increase in size very quickly are not usually dangerous
As I said, the above are not hard and fast rules. All lumps should be assessed by a medical professional, especially if you have never had a lump before.
Many breasts become lumpy before menopause. This is due to changes in hormone levels. However, as women age they are at higher risk of developing breast cancer, so if you are close to menopause you should not assume that lumps in your breasts are normal. Danger signs that warrant immediate attention and concern include changes in the skin (dimpling or thickening), a change in the size or appearance of a breast or a change in the nipple position (including inversion of the nipple). Nipple discharge (clear, sticky or blood-tinged fluid) should also be checked carefully by a physician.
As I mentioned earlier, many women discover their own lumps while showering. Partners also sometimes discover breast lumps. It is important for women to check their breasts regularly (men should also examine their testicles for lumps routinely). Get in the habit of checking your breasts for lumps on a monthly basis. Breasts should be examined in the shower (soap helps the fingers glide smoothly over the skin). The pads of the fingers should be used to check the entire breast, moving from outside to the inside, checking the entire breast (don’t forget the armpit). Breasts should also be examined in the mirror with your arms at your sides and raised above your head. This helps you to see any obvious changes in shape or size (note that it is normal for one breast to be slightly larger). Lastly, examine your breasts while you are laying down, which allows the breast tissue to spread out along the chest wall. You should move the pads of your fingers in small circles, being sure to cover the entire breast. You should also be sure to squeeze the nipple to check for discharge.
Up to 40% of breast cancers are discovered by women, not their physicians, so get in the habit of checking your breasts monthly. If you find a lump or notice a change in one of your breasts, make an appointment and come in to see me. I can determine fairly quickly whether the lump is cause for concern and, if it is, refer you for further testing or a second opinion. You can combine your visit with a pap smear if you are due (or overdue) for your exam.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.
Answer: Every year, my patients ask me this question, so thank you for bringing this important topic to the forefront!
Flu season will be upon us soon. Typically, the influenza vaccine is made available to doctors by mid to late October. This allows us to immunize a large proportion of the population before flu season hits hard, which usually coincides with the holiday season when people gather together in large crowds indoors- this practice helps to spread the virus very efficiently! It takes a few weeks for the flu shot to take full effect, so immunizing in the fall makes sense.
Many people question the need for a flu shot. In order to understand why I advocate getting a flu shot, it’s important to explain the concept of herd immunity. This term refers to the fact that when a large proportion of individuals are vaccinated against a certain disease, those who cannot be immunized (such as small children or people with compromised immune systems) will still enjoy a measure of protection. In other words, the more people get vaccinated, the greater the chance that susceptible individuals who may die from the disease in question will be protected. The concept of herd immunity explains why we are seeing a resurgence of diseases such as diphtheria and measles. Many parents are choosing not to immunize their children, and as fewer people are immunized, these diseases are becoming more commonplace again.
Many healthy adults are resistant to the idea of immunization against the flu, claiming that they never get the flu and, at any rate, they are healthy and should have no problems recovering if they do get it. Many people forget that influenza can result in significant illness, even in people who are healthy with no chronic health issues. Even if you are healthy, getting the flu can mean that you are too weak and sick to get out of bed for several days, which means time off work and lost pay for some. Can you afford a week away from work or school?
If you have contact with children or older adults, getting the flu shot may protect them. The flu claims many lives every year (which many people seem to forget), and getting the flu shot may be the best way to protect those you care about from getting ill.
If you have a chronic health condition, you should definitely get a flu shot. Anyone with heart and/or lung disease, obesity, diabetes or other chronic conditions should get a yearly flu shot, as getting the flu could result in serious complications. If you are an older adult, you are at higher risk of complications such as pneumonia.
To answer your question, I believe that everyone should get a flu shot to protect not only themselves, but others who are high risk of dying from the flu, such as infants, patients fighting cancer or other serious illnesses affecting their ability to fight off infection and the very old.
Back to Q & A
Our Location

6301 Mill Lane, Brooklyn, NY 11234.
Answer: People get confused between the common cold or the flu all the time. The flu and a cold share common symptoms but are not the same. The flu generally makes you far sicker for a longer period of time than the common cold does.
-
Onset– the flu hits quickly. You may wake up in the morning feeling well and by afternoon you may be so sick that you have no choice but to go to bed. A cold comes on slowly. It may start with a tickle in your throat and a runny nose and progress over a couple of days until symptoms are full-fledged.
-
Fever– with a cold, you may experience a low-grade temperature. With influenza, you may get chills and a very high temperature.
-
Muscle aches– with a cold you may feel unwell and you may feel a little achy. When you get the flu, you may experience intense muscle aches all over your body.
-
Ability to work – most people who have a cold are able to continue working (this is not to say that they should, only that most can). With influenza, the affected person may be so weak and ill that they will find it impossible to work (and they should definitely not go to work and spread the virus to others!)
-
Coughing – both influenza and the common cold are respiratory illnesses. A cold will often lead to a cough that may be productive. The cough associated with influenza is dry and non-productive.
-
Sore throat – sore throat may be one of primary symptoms with a cold and may be very uncomfortable. You may also experience a sore throat with influenza but it will not be the primary symptom.
-
Nausea and vomiting – nausea and vomiting is not a common symptom with either illness, but some people with influenza may experience nausea and vomiting and possibly even diarrhea, depending on the flu strain. For example, the H1N1 strain of influenza that hit so hard in 2009 caused gastrointestinal symptoms in a larger proportion of sufferers than is typically seen with the flu.
-
Nasal congestion – this is very common with a cold. It is far less common with the flu.
-
Headache – headache is very common with influenza. It may occur in the common cold but is less common and is usually not severe.
-
Complications – complications may occur with either illness. Otitis media (middle ear infection), bronchitis and sinus infections may occur as a consequence of the common cold. With influenza, pneumonia is not uncommon and may be deadly for the elderly and those with compromised immune symptoms. People with underlying lung disease may experience a complication of either illness more often than people who have a health respiratory system and the ability to fight off infection.
Washing your hands is the most important thing you can do to stay well this winter. You cannot wash your hands too often! To avoid the flu, I strongly recommend that you get a flu shot, particularly if you are obese, you are a smoker or you have a chronic health condition such as diabetes, heart disease or lung disease. If you are taking medications (such as steroids) that can weaken your ability to fight off infection or if you are being treated for a chronic health condition, getting a flu shot may be life-saving.
Back to Q & A
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

The symptoms of inflammatory bowel disease can be debilitating and can negatively impact quality of life. If you have inflammatory bowel disease, you will need a physician who can coordinate your care with a gastroenterologist and work with you to manage your condition, so that you can live as symptom free as possible!
-Dr. Zimilevich, MD
What is inflammatory bowel disease (IBD)?
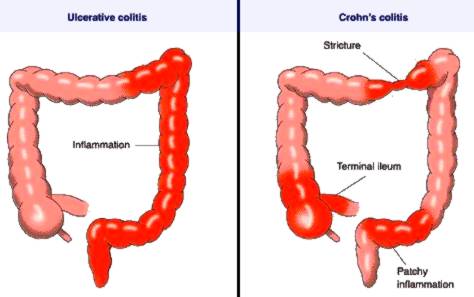
In inflammatory bowel disease, parts of the bowel become inflamed. There are two main types of IBD:
- ulcerative colitis- ulcerative colitis usually develops slowly over time and involves continuous segments of the rectum and colon (large intestine). Usually the innermost lining is affected.
- Crohn’s disease- in Crohn’s disease, inflammation may occur anywhere in the small and large intestines. Inflammation may involve deep layers of the bowel
What are the symptoms of inflammatory bowel disease?
Symptoms are a little different for ulcerative colitis and Crohn’s disease, although they may share some symptom:
- ulcerative colitis- symptoms of ulcerative colitis may vary according to the areas of the large bowel affected. Symptoms are mildest when only the rectum is involved, causing rectal pain, bleeding and a sense of urgency surrounding bowel movements (ulcerative proctitis). Sometimes rectal bleeding is the only symptom experienced. When greater segments of the colon is involved, symptoms may include bloody diarrhea, abdominal pain and cramping, tiredness and unintended weight loss. Bouts of illness may alternate with periods of wellness (remission).
- Crohn’s disease- in addition to abdominal pain and cramping, diarrhea, blood in the stool, decreased appetite and malnutrition due to the inability of diseased bowel to absorb nutrients (remember, the small bowel can be involved in Crohn’s, which is where nutrients are absorbed), Crohn’s is a systemic disease that can affect other body systems. Individuals with Crohn’s may also have fever, rashes, fatigue, arthritis and inflammation affecting the eyes. As with ulcerative colitis, people with Crohn’s disease may experience periods of remission when their symptoms disappear.
What causes inflammatory bowel disease?
No one really knows. Researchers believe that both disorders may be an autoimmune response. It is also possible that heredity may play a role, as people who have family members with IBD are more likely to develop one of these disorders.
Risk factors for IBD include:
- age- most people with IBD are under the age of 30, but IBD develops later in some individuals (50s and 60s)
- cigarette smoking- smoking can make your symptoms worse and increases the risk of complications
- NSAID use- using non-steroidal antiinflammatory agents, such as ibuprofen or Naproxen, can cause ulceration in the GI tract and may worsen IBD. Tylenol is safe to use.
- ethnicity- Caucasians and people of Jewish descent have a higher prevalence of IBD
- family history- as mentioned, having someone in your family diagnosed with the condition raises your risk

What can I expect when I come to see you?
When you come in to see me with gastrointestinal symptoms that suggest inflammatory bowel disease, I will need to know a little about your past medical history, your family medical history and what drugs you are currently taking, if any.
Next, I’ll ask you about your symptoms. I may ask you about:
- pain- where is it located? does it come and go? is the pain related to bowel movements? on how many days of the past month did you experience abdominal pain?
- bowel habits- are you experiencing diarrhea? constipation? how often do your bowels move and what is the consistency of your bowel movements?
- blood in the stool- is there fresh blood only when you wipe, is the blood mixed in the stool, or is there blood in the toilet water?
- weight loss- have you lost weight unintentionally? how much weight do you estimate you have lost?
- fever- have you been experiencing any fever?
- other symptoms- have you experienced other symptoms, such as rash, joint pain or eye inflammation?
Although these questions may make you squeamish, remember that the more information I have, the better and more accurately I can diagnose you. Please don’t feel embarrassed- I am a doctor and chances are I have heard it before!
I will need to examine you and may ask you to change into a gown. I may weigh you to get a baseline weight. I will listen to your abdomen for abnormal bowel signs. I will also gently press your abdomen in several places to see if I can feel any abnormal masses and to determine what areas are tender when I press on them.
I will likely order diagnostic tests, such as blood work to check for anemia and inflammation, as well as malnutrition if you have lost weight. I may order an abdominal x-ray. If I feel your symptoms are consistent with inflammatory bowel disease, I may order a colonoscopy, which is a test that uses a scope to view the inside of the bowel (you are sedated throughout the exam). If necessary, I will refer you to a gastroenterologist.
If you are suffering with symptoms that may be IBD, you need to come in and see me as soon as possible. The longer you wait, the more damage that may be done to your intestines. Don’t delay- make an appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Abdominal pain can have numerous causes. It can be difficult even for doctors to differentiate between serious and benign causes of abdominal pain. The abdomen contains many organs that can potentially cause problems. For this reason, it is always best to err on the side of caution. Most of the time abdominal pain is not serious, but when it is serious it is VERY serious. If you are experiencing abdominal pain, come in and see me.”
-Dr. Zimilevich, MD
What is abdominal pain?
Abdominal pain is any pain that occurs below the xiphoid process (the bottom tip of your sternum or breastbone) and above the pubic bone. It may be dull, sharp, constant, intermittent, stabbing or aching in nature. It may occur on its own or may be accompanied by other signs and symptoms, such as nausea and vomiting or fever. These accompanying signs and symptoms can provide clues as to what may be causing the problem.
What causes abdominal pain?
Abdominal pain can be caused by many issues affecting the organs found in the abdominal cavity, including:
- gynecological problems- in women pain may arise from problems affecting the uterus, ovaries or fallopian tubes
- the stomach- stomach viruses, food poisoning and ulcers are common problems affecting the stomach. Invariably, appetite will be affected. Nausea and vomiting may also occur. Pain in the stomach is often referred to as burning or gnawing pain. Chronic issues affecting the stomach may result in weight loss.
- the intestines- intestinal illnesses can cause a lot of discomfort. Pain may be constant or intermittent and may be sharp or dull. There may be accompanying signs and symptoms such as nausea, vomiting, blood in the stool, weight loss, rectal pain, inability to pass flatus (gas or wind) or fever. The location of the pain can also provide clues. Pain that is centered around the belly button is likely to be caused by a problem in the small bowel; intestinal pain arising from the large bowel may be felt all over as generalized tenderness. History and physical exam will provide other clues. Intestinal problems may be infectious (a viral or bacterial cause such as food poisoning), may be caused by inflammatory bowel disease, adhesions or blockage of the bowel.
- the appendix- the appendix is located in the right lower quadrant of the abdomen. Pain often begins around the belly button and may eventually move to the right lower side of the abdomen, midway between your hip bone and your belly button, known as McBurney’s point. If you have appendicitis, you will not have an appetite and you may be constipated. You may have a low-grade fever. Pain gradually worsens over time. Appendicitis is a surgical emergency. If you have symptoms of appendicitis, you should seek medical attention immediately.
- the pancreas- pancreatitis (inflammation of the pancreas) causes severe pain that will be difficult to ignore. The pain occurs in the upper abdomen and may radiate through to the back. Pancreatitis may also cause nausea and a low-grade fever. People with pancreatitis feel very ill. Gall stones or alcohol may precipitate an attack of pancreatitis.
- the gallbladder- gallstones or infection of the gallbladder can cause severe pain that is usually felt in the upper abdomen and may radiate to the back. Gallstones may block the bile duct, causing intense pain that may occur after eating a heavy or fatty meal. The pain usually subsides within a few hours but may reoccur again. Nausea and vomiting may occur.
- urinary tract problems- infection in the urinary tract (bladder or kidneys) may cause abdominal pain. Kidney infection or stones often cause severe pain that is felt in the flank area (just below the ribs and beside the spine on the affected side). Nausea and vomiting may occur. Fever will occur with infection. Testing the urine may reveal infection or blood in the urine.
- diverticular disease- the colon may develop weakened areas of the muscular wall that bulge out, allowing waste to collect in these areas. When these pockets develop infection, symptoms will include lower left abdominal pain, fever and flu-like symptoms. Diverticulitis requires antibiotics.
These are some of the common problems that may cause abdominal pain- there are many more. As you can see, the many organs of the abdomen present a challenge to diagnosis!
E
What can I expect when I come in to see you?
When you come in to see me with abdominal pain, I will first ask you about your past medical history, including any surgeries you may have had. I will also ask about family history and medications you are taking.
I will ask you about your symptoms. When did they start? Where is the pain? What is the nature of the pain (i.e. sharp or dull)? Is the pain constant, or does it come and go? Does the pain radiate (move) to other areas? What other symptoms are you experiencing (i.e. diarrhea, vomiting, fever)?
Once I have a handle on your symptoms, I will examine you, focusing on your abdomen. I will listen to your bowel sounds. I will also palpate (feel) your abdomen for areas of tenderness, swelling or masses. I will be paying attention to where your abdomen hurts the most. Once I have examined you and discussed your symptoms, I will likely order tests, which may include blood tests, an abdominal x-ray and urinalysis. I may order other tests as I see necessary.
Based on all of the information gathered, I will probably have a good idea as to what may be causing your abdominal pain and we can discuss what treatment is necessary to relieve your pain. If I cannot determine the source of your pain, I may refer you to a gastroenterologist.
If you are experiencing abdominal pain, make an appointment to see me. Some conditions that cause abdominal pain are benign, but others may be very serious and require immediate care. Make your appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Trigeminal neuralgia is an extremely painful condition affecting the nerves of the face. If you have symptoms of trigeminal neuralgia, don’t despair- help is available.”
-Dr. Bella Zimilevich, MD
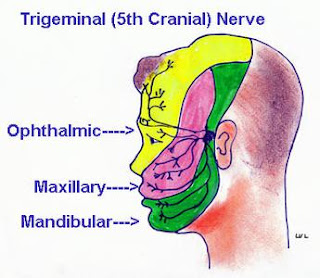
What is trigeminal neuralgia?
The trigeminal nerve is a nerve in your face that carries nerve sensations from your face to your brain. In trigeminal neuralgia, this nerve malfunctions, so that the mildest forms of stimulation of the nerve (i.e., applying makeup, brushing your teeth) can cause excruciating pain.
Trigeminal neuralgia often starts with short episodes and progresses to longer and more painful episodes. The condition often affects older people, and women are affected more often than men. Although trigeminal neuralgia is extremely painful, treatment is available- you don’t need to be afraid that the pain will haunt you forever.
What are the symptoms of trigeminal neuralgia?
Symptoms of trigeminal neuralgia include:
- pain in the area supplied by the trigeminal nerve (teeth, lips, gum, jaw and sometimes the forehead and/or eye)
- pain triggered by chewing, talking, smiling, shaving, brushing your teeth, applying makeup or touching your face
- pain on one side of your face
- pain focused in one particular area or spread out over a wider area
- pain that begins as occasional mild twinges, progressing to episodes that are more painful and longer lasting
- episodes of pain lasting days, weeks, months or longer
What causes trigeminal neuralgia?
Trigeminal neuralgia is thought to occur when pressure is placed on the trigeminal nerve by a vein or artery at the base of the brain. This pressure causes the trigeminal nerve to malfunction. Sometimes a lesion such as a tumor applies pressure to the nerve, and sometimes MS, a condition in which the myelin sheath that protects our nerves becomes damaged. Many times a cause for trigeminal neuralgia cannot be found. The condition is more common after age 50, so aging may play a role.
What can I expect when I come to see you?
When you come to see me, I will first ask about your health history, your family’s health history, any medications you are taking and whether you have any allergies.
I will ask you the following:
- When did your symptoms start?
- How long do symptoms last? Do they come and go, or is the pain constant?
- What activities seem to trigger your pain? (i.e., talking, eating, smiling, touching your face)
- Have you ever had any facial trauma or surgery near the area where you are experiencing pain? (i.e. dental or sinus surgery)
- What have you tried to ease the pain? Was it effective?
- Do symptoms affect one or both sides of your face?
- Are symptoms getting worse over time?
- How does the pain affect your quality of life?
The answers to these questions will provide me with a lot of needed information so that I can make a proper diagnosis. I will also examine you, including the area where you are experiencing pain. If my examination causes pain, please be sure to tell me. If necessary, I will order an MRI to help me make the diagnosis. We can discuss the need for an MRI if one becomes necessary.
How is trigeminal neuralgia treated?
Medications are used first and are very effective for many people. The two main classes of drugs used are anticonvulsants (used for the nerve pain, not to prevent seizures) and antispasmodic drugs. These medications may have side effects such as drowsiness which will pass with time.
Should medications prove to be ineffective in treating your pain, I can refer you to a neurologist, who may suggest surgery to decompress the nerve, or injections that damage the trigeminal nerve so that it can no longer process pain signals. These procedures are not without risk and should be discussed with your neurologist. If you see a neurologist, I can work with your neurologist to treat you.
If I suspect that something other than trigeminal neuralgia is causing your pain, I may order other tests.
If you suffer from facial pain, make an appointment to come in to the clinic to see me. I can help you get to the root of the problem and treat your pain. Don’t delay- make an appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Angina is not a disease in and of itself; instead, it serves as a warning that an area of the heart is not getting enough oxygen. Angina should never be ignored- you should take it as the warning that it is and seek medical care if you experience chest pain or discomfort.”
-Dr. Bella Zimilevich, MD
What is angina?
Angina is chest pain or discomfort that occurs when a portion of the heart does not receive enough oxygen-rich blood. It usually occurs due to coronary artery disease (CAD). If you have CAD, an artery (or more than one artery) becomes partially blocked with plaque, a waxy substance that can occlude arteries and block blood flow. High cholesterol can influence plaque formation, and high blood pressure can damage arteries, making them stiffer and less pliable, and thus less able to allow blood to flow freely. When plaque builds up, a clot can form, which can increase your risk of having a myocardial infarction (heart attack) if a clot happens to occlude an artery, completely blocking the flow of blood in the affected artery.

What are the types of angina?
Angina can take more than one form. It is important to determine which type of angina you have, as treatment may vary:
- Stable angina– this is the most common type. In stable angina, the heart must work harder than normal to do its job, and anything that increases the workload of the heart may cause pain. In stable angina, you can usually predict what activities will provoke pain. The pain subsides when you rest or take your medication. Stable angina is a warning that a heart attack may occur in the future.
- Un
 stable angina– unstable angina occurs not only during activity, but also at rest. Unstable angina is unpredictable and may not stop when you rest or take medication. Unstable angina is a warning that a heart attack may be imminent and should be taken very seriously.
stable angina– unstable angina occurs not only during activity, but also at rest. Unstable angina is unpredictable and may not stop when you rest or take medication. Unstable angina is a warning that a heart attack may be imminent and should be taken very seriously.
- Variant angina– this type of angina occurs when a coronary artery goes into spasm. It is very painful and often occurs in the middle of the night. It can often be controlled with medication.
Is all chest pain caused by angina?
No. Chest pain can be caused by many other conditions other than angina. This is why it is so important to see a doctor if you are experiencing chest pain. Chest pain can be caused by musculoskeletal injury to the chest wall, pulmonary embolism, pneumonia and other conditions, some of which may be very serious and some, like musculoskeletal injury, that are painful but not life-threatening.
What can I expect when I come and see you?
If you come in and see me with chest pain, I will ask about your past medical history, medications you are taking and any allergies you might have. I will also ask about your family history of heart disease.
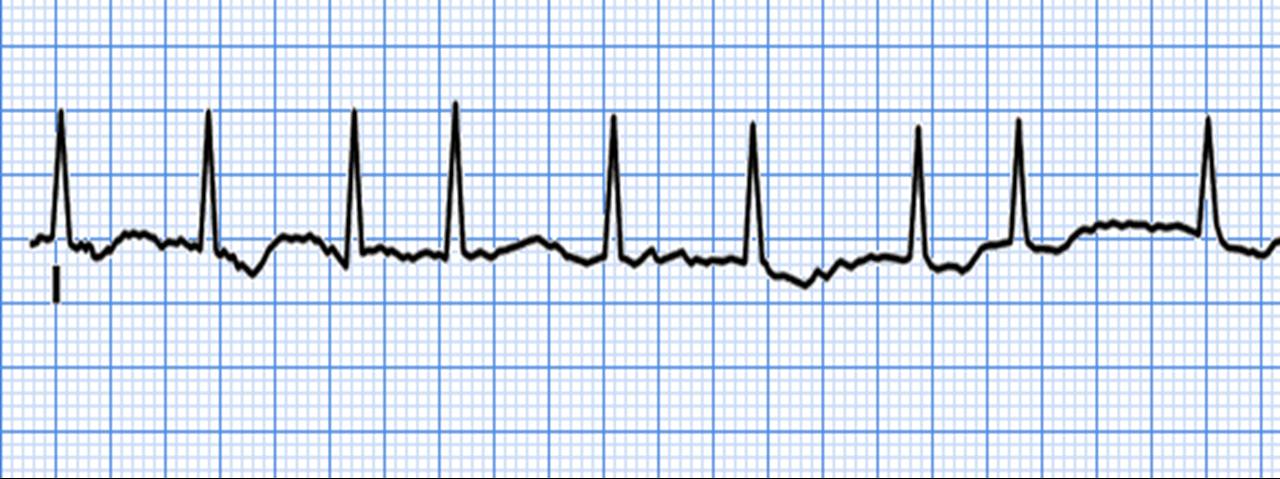
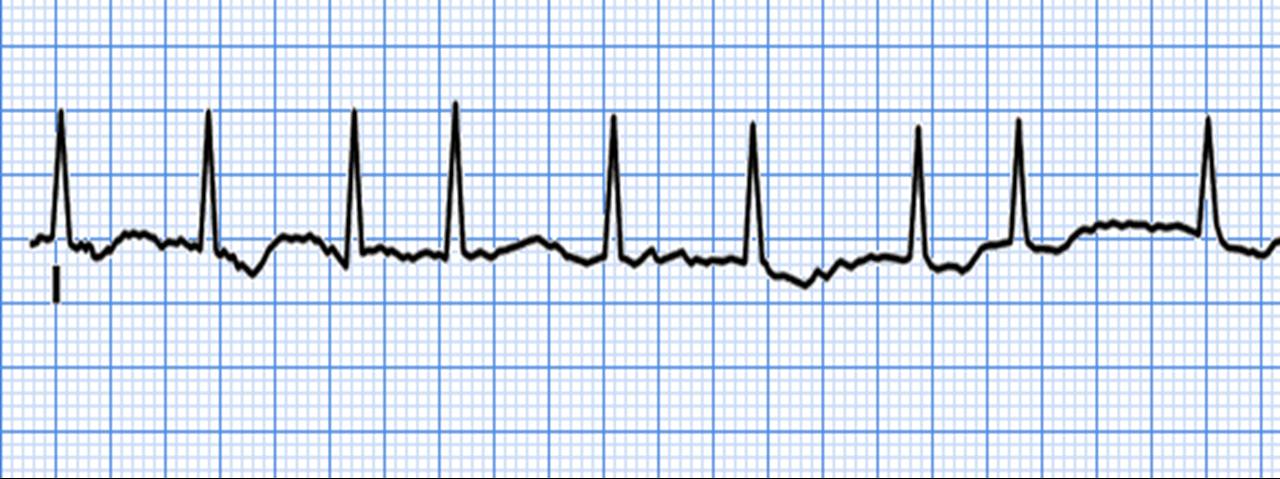
I will examine you, paying close attention to your heart and lungs. I will order an ECG, which records the electrical activity of your heart and can tell me if you have an abnormal rhythm or if you have ECG changes that indicate your heart is not getting enough oxygen (“ischemic changes”). I will also check your blood pressure and other vital signs. I may order blood tests, depending on what I think the cause of your chest pain might be. Blood tests might include a complete blood count, cholesterol testing and other tests that will provide me with information regarding your general health status. I may also order a stress test, which measures how well your heart functions under “stress” (exercise).
If need be, I may refer you to a cardiologist if I feel you need to see a specialist. I can work with your specialist and you to ensure that your care needs are being met.
If you have angina or chest pain, don’t wait to come in to be seen. Chest pain should always be assessed by a medical professional to rule out cardiac disease or other serious conditions. If you have chest pain, don’t delay- make an appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Atrial fibrillation is a relatively common cardiac arrhythmia in older patients. Although it is common, it should not be ignored, as it can lead to serious complications such as stroke. If you have symptoms of atrial fibrillation, it is important that you come in immediately to be seen”.
-Dr. Bella Zimilevich, MD
What is atrial fibrillation?
Atrial fibrillation is an abnormal rhythm of the atria, the upper chambers of the heart. In atrial fibrillation, instead of the atria contracting regularly and forcefully in concert with the ventricles, sending blood to the ventricles where it can be pumped out to the rest of the body, the atria quiver chaotically (and often very rapidly), resulting in decreased blood flow to the ventricles. This can cause fluid to back up into the lungs, causing symptoms of congestive heart failure. Atrial fibrillation is also a major risk factor for stroke. Why? When the atria quiver, blood can coagulate and form a clot, which may then be pumped out into the circulation and may eventually head for the brain, causing a stroke. Atrial fibrillation may be acute or chronic.
What are the symptoms of atrial fibrillation?
Some people are not aware that they have atrial fibrillation and do not notice that their heart is beating irregularly. Others, especially people who have chronic heart disease such as congestive heart failure, may experience:
- palpitations, the sensation that their heart is beating irregularly or too quickly or is “flopping around” in their chest
- shortness of breath
- lightheadedness/weakness
- chest pain
- low blood pressure
- confusion (due to lack of oxygen to the brain)
- chest pain (Note: if you have chest pain and/or severe shortness of breath and palpitations, you should go to the nearest emergency room, as chest pain may indicate that you are having a heart attack. It’s always better to be safe than sorry.)
Paroxysmal atrial fibrillation may come and go. Chronic atrial fibrillation means that your heart rhythm is always irregular.
What causes atrial fibrillation?
Atrial fibrillation may occur in conjunction with, or because of, many other conditions:
- previous heart attack- a previous heart attack may damage tissue that is normally responsible for regulating heart rhythm
- diseased heart valves- heart valves that do not open and close properly, allowing blood to flow backwards in the heart (regurgitation) may cause atrial fibrillation
- thyroid disease- if your thyroid is overactive, you may experience paroxysmal atrial fibrillation that can usually be treating your hyperthyroidism appropriately
- high blood pressure- high blood pressure can damage the heart over time
- congenital heart defects- if you are born with abnormalities of the heart, you may develop atrial fibrillation
- lung disease- emphysema and COPD may cause atrial fibrillation
- stimulants- caffeine, alcohol, tobacco or certain drugs may cause transient atrial fibrillation that will go away once the offending substance wears off
- malfunctioning of the normal pacemaker of the heart (the SA node, which normally regulates heart rate)
What can you expect if you come and see me?
If you are experiencing symptoms such as palpitations, weakness, dizziness or shortness of breath, it’s very important that you be seen by a physician. Ignoring these symptoms may mean that you could suffer a stroke or other complication.
When you come to see me, I will ask you about your past medical history, looking for clues as to what may be causing your symptoms. I will want to know about all the medications you are taking, including over-the-counter and herbal remedies. I will also want to know if you have any allergies to medications.
I will need you to tell me in detail about your symptoms: When did they start? Do they come and go? Does anything make them better or worse? Be as specific as you can and tell me everything, even if you think it is not relevant.
After I have gathered some information, I will examine you. I will listen carefully to your heart and lungs. I may also assess your legs and abdomen for edema (excess fluid that has pooled in your legs or abdominal area). I will obtain your vitals (heart rate, blood pressure, oxygen saturation). I may also weigh you so that we have a baseline for comparison in the future.
I will order an ECG, which is a recording or your heart’s electrical activity. The test is not painful and takes only minutes to perform. It can provide valuable information on the condition of your heart. I may also order blood work, including a complete blood count and electrolytes to check for electrolyte imbalance and anemia, as well as liver function tests, cholesterol tests and others as I feel they are necessary.
If you have atrial fibrillation, we can talk about treatment. If I feel it is necessary, I may send you to a cardiologist. If you need to be seen by a heart specialist, I will work with your specialist to care for you, following your specialists’ recommendations. If you have atrial fibrillation, it will be important for you to be seen regularly in order to keep on top of your condition and prevent serious complications.
How is atrial fibrillation treated?
Treatment is aimed at prevention of blood clots and control of your heart rate. This is usually achieved with medications such as blood thinners and heart medications that slow your heart rate. Treatment will depend on how long you have had symptoms, how much your symptoms bother you and what the underlying cause of your atrial fibrillation is thought to be.
If you have symptoms of atrial fibrillation, do not ignore your symptoms. Make an appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Sprains and strains can be very painful. When treated properly, the swelling and pain should diminish quickly. However, doing too much too soon may result in reinjury. It can be difficult initially to tell the difference between a bad sprain and a fracture, in which case it may be necessary to seek a professional opinion”.
-Dr. Zimilevich, MD
Sprains and strains- what is the difference?
Although the terms sound similar, sprains and strains are not the same. A sprain involves injury to the ligaments that connect bones together at the joint, while a strain is an injury to a tendon or muscle. The most common sprain is the ankle sprain, while back injuries are a common form of muscle strain.
What are the signs and symptoms of sprains and strains?
If you experience a sprain, you will notice bruising, swelling, pain and a limited ability to move the affected joint. You may feel (or even hear) a loud “pop” when the injury occurs.
If you sustain a strain injury, you may notice swelling, pain and a limited ability to move the affected muscle. You may experience painful muscle spasms.
What causes sprains and strains?
A sprain occurs when you overextend your ligament while placing stress on the joint. The tendon may actually tear. A strain occurs when the muscle is stretched beyond its normal capacity. Strains may be acute or chronic. While acute strains occur suddenly, usually as the result of a single event or moment, acute strains may occur when a muscle is strained repetitively.
Who is at risk of suffering a sprain or strain?
If you are in poor condition and stress your ligaments or muscles beyond what they are capable of, you may injure them. If you are in good condition but fail to warm up your muscles adequately before engaging in physical activity, you may experience an injury. Becoming overly fatigued may also result in injury as you are less likely to protect your joints. Sometimes sprains and strains are the result of an accident that can’t be prevented.
How do I know if I need to come see you?
If you are unable to walk without a great deal of pain, or you cannot bear any weight on the affected joint, you need to come in and see me. If you have numbness in the injured area or you cannot move the affected joint, it is important to have you injury evaluated.
What can I expect when I come in to see you?
When you come in to see me, I will first gather a little history about you, including your past medical history, medications you are taking and any allergies to medications you may have.
Next, I will need you to tell me how the injury occurred. I will need to know what you were doing when the injury occurred (playing a sport, shoveling the sidewalk). How long have you had the pain? Have you ever injured the same area before? Did you hear or feel any noises when the injury occurred? The answers to these questions can provide me with some clues to help make the diagnosis.
I will then examine the affected area, looking for bruising, swelling and pain with gentle manipulation of the joint, as well as range of motion. After I have examined the joint, I will determine whether the area needs to be x-rayed to complete my evaluation.
How do you treat sprains and strains?
Treating a sprain or strain involves RICE:
- Rest- rest the affected area
- Ice- apply ice to the area for 10 to 15 minutes 3 times/day
- Compression- wrap the area with an ace bandage (support bandage), being careful not to wrap the area too tightly
- E– elevate the affected area if possible above the level of your heart to decrease swelling (i.e. put your ankle up on a chair while you are sitting)

Over-the-counter analgesics such as ibuprofen or Tylenol can be used as directed for pain. Crutches may be necessary for severe ankle or knee sprains.
If you are unable to work due to your injury, I can provide you with a note for work. If you injured yourself on the job and your injury is a Workman’s compensation claim, please let my office staff know prior to your visit so that we can help you complete the appropriate paperwork.
If you have suffered a sprain or a strain and you are unable to walk or bear weight, or you experience numbness in the area, make an appointment to see me urgently. In most cases, you can be seen on an urgent basis. Make your appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“COPD is a condition that requires careful maintenance to prevent exacerbations (flares) of the disease. If you have COPD, you need a physician who can help you manage medications and prevent flares. As your primary care physician, I will be committed to keeping you as healthy as you can be”.
-Dr. Zimilevich, MD
What is COPD?
COPD, which stands for chronic obstructive pulmonary disease, is a chronic lung disease that includes emphysema and bronchitis. Some people with COPD have both conditions. Smoking is a major cause of COPD, but non-smokers can also develop COPD. COPD causes damage to your airways which carry oxygen to and from your lungs. Your airways can become swollen and blocked by increased mucous production (bronchitis). In addition, the tiny air sacs in the lungs where oxygen exchange takes place become damaged (emphysema), making it difficult to breathe.
What are the symptoms of COPD?
Symptoms of COPD develop gradually. Symptoms may include:
- chronic cough
- coughing up phlegm (mucous)
- shortness of breath on exertion (and sometimes at rest in advanced stages)
- weight loss
- wheezing
- frequent chest infections that take a long time to clear up

How is COPD diagnosed?
I can make the diagnosis of COPD based on my physical examination, a chest x-ray and spirometry, a pulmonary function test which measures how well you can move air into and out of your lungs. Blood tests such as arterial blood gases may also be useful in helping me to make the diagnosis.
What can I expect when I come to see you?
When you come to see me with breathing concerns, I will first ask you about your past medical history, including any history of lung infections such as pneumonia. I will ask you about any medications you are taking and also about any allergies you may have. I will also want to know if you have a family history of lung disease such as COPD or asthma.
Next I will ask about specific symptoms, such as coughing and shortness of breath. I will need to know if you are always short of breath, or if you are short of breath only when exerting yourself. If you are coughing frequently, are you bringing up any mucous? Do you wheeze when you exert yourself? Do you have frequent colds or chest infections that seem to take a long time before they get better? Do you suffer from chronic fatigue, or have you lost weight unintentionally?
I will ask you about your smoking history. Many patients feel the need to downplay their smoking history, or deny it outright. Remember that I am not here to judge, only to help. If you do have COPD, quitting now can make a world of difference in terms of the progression of the disease. I would be happy to discuss quitting options for you, including prescription medications or patches available.
Next, I will examine you. I will focus on your heart and lungs, listening carefully to both. People with COPD may have congested lungs or wheezing breath sounds. I will also check your vital signs, including your oxygen saturation. I may order a chest x-ray, spirometry and any other tests I feel are necessary to help me make a diagnosis.
How do you treat COPD?
First of all, if you are a smoker, I must urge you to quit. It’s never too late to quit! You can dramatically influence the course of your disease by quitting smoking. This fact cannot be emphasized enough. I understand that smoking is perhaps one of the hardest habits to break, and I will be here to support you using whatever tools you need to help you achieve your goal of becoming a non-smoker. You can do it!
Medications are used to keep you feeling your best and prevent flare ups of the disease. You may take a daily bronchodilator to keep your airways open and allow you to be at your best. Steroids may be used for exacerbations, and antibiotics may be needed at times if you have a chest infection. It is very important that you understand your medications- what they are used for and how to take them properly. We will spend time together discussing any medications I prescribe.
Exercise is important if you have COPD. If you exercise, your heart and lungs benefit, and you may be able to stave off a decline in your breathing. Any kind of exercise is helpful. Walking is very beneficial. We can talk about what types of activities you enjoy and can engage in to maintain your pulmonary health.
Some people with chronic diseases such as COPD lose weight because their bodies require more energy to perform normal activities. Eating a healthy diet is important to prevent exacerbations in COPD. You can follow the American Heart Association’s Heart Smart diet. Feel free to ask me any questions about diet and how a healthy diet can benefit you.
From time to time you may benefit from seeing a pulmonary specialist. If necessary, I can refer you to a specialist in lung disease, and I can work with you to follow your specialist’s recommendations. It is important that you have one doctor to act as the “gatekeeper” for your health, someone who knows all about you and who you can see regularly for all health concerns, not just those relating to COPD. I would love to be your partner in managing your health. Together, we can help you to enjoy good quality of life and prevent flares.
If you are concerned that you may have COPD, or you have COPD and are searching for a primary care physician to oversee your health, please call the clinic to make an appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Irritable bowel syndrome (IBS) is a condition causing abdominal discomfort and is a common reason for seeking medical care. If you suffer from abdominal pain and cramping combined with altered bowel habits (diarrhea, constipation or both), you should make an appointment to come in and see me so that we can determine if you have IBS. These symptoms are also common in other, more serious conditions so it is important to rule out other conditions as well”.
-Dr. Bella Zimilevich, MD
What is irritable bowel syndrome (IBS)?

IBS is a collection of symptoms caused by a change in how the bowel functions. It is not a disease; in other words, the structure of the bowel itself does not change. Functional disorders of the gastrointestinal tract cause real symptoms. Just because there is no actual damage to the gastrointestinal tract does NOT mean that your symptoms are not real- the symptoms of IBS are all too real and can be quite distressing for some. IBS causes alterations in bowel function, along with abdominal bloating and other symptoms. Women are affected more often than men, and the condition is diagnosed in younger people more often than in older people.
Types of IBS
IBS can be classified according to the predominant symptom:
- IBS-C (IBS with constipation)- people with IBS-C experience constipation more often than diarrhea, although both may occur
- IBS-D (IBS with diarrhea)- people with IBS-D experience diarrhea more often than constipation, although both may occur
- Mixed IBS- people with Mixed IBS experience both diarrhea and constipation at least 25% of the time
IBS is usually diagnosed if you experience symptoms of abdominal pain at least 3 times a month that cannot be explained by another condition. Abdominal discomfort may be relieved by a bowel movement and may be associated with a change in your bowel movements.
What are the symptoms of IBS?
The primary symptoms of irritable bowel syndrome are abdominal discomfort and a change in bowel habits. Symptoms must occur more than 3 times a month to meet the criteria for IBS. Pain is associated with one of the following:
- more frequent/less frequent bowel movements
- stools that are harder than usual or more watery/loose than normal
- relief with a bowel movement (pain goes away after a bowel movement)
You may also experience abdominal bloating (often worse after eating), the sensation of incomplete emptying of the bowel/rectum and mucousy (but never bloody) stools.
What causes IBS?
Researchers are not 100% sure what causes IBS. Stress may play a role- you may find that your symptoms are worse during times of physical or emotional/mental stress. Overgrowth of bacteria in the gut has also been blamed for IBS. Poor motility (the ability of your intestines to move food along the intestines) has been postulated as causing IBS. Food sensitivity and hormones (IBS is often worse during menstruation) are other possible causes.
What can I expect when I come to see you?
When you come to see me and you are worried about IBS, I’ll begin by asking you a lot of questions. I’ll ask about:
- past medical history, including abdominal surgeries
- medications you are taking
- allergies to foods or medications
- family history of gastrointestinal disease
- whether you have had any fever, blood in your stool, weight loss or other symptoms suggestive of colon cancer or an intestinal infection
- whether you have traveled recently
I will need to know how long you have had symptoms, when your symptoms started and how often you experience symptoms. I will also ask about your bowel habits (how often you have a bowel movement). If you are a woman I may also ask about your menstrual pattern and whether symptoms are associated with your period.
Once I have gathered all of this information, I will examine your abdomen to feel for any tender areas or masses. I will listen for bowel sounds. If necessary, I may order diagnostic tests, such as blood work to check for anemia or infection or stool studies to check for bacteria or parasites in your stool. I may order other tests such as an abdominal x-ray or abdominal ultrasound as necessary. Quite often the diagnosis of IBS can be made without the need for a lot of tests, but it is also important to rule out other serious causes of your symptoms such as bowel cancer or inflammatory bowel disease.
Once I have all of the information I need, I will be able to tell you what I think may be causing your symptoms. If I am unable to determine the cause of your symptoms, I will refer you to a specialist (a gastroenterologist). This is rarely necessary.
What is the treatment for IBS?
Treatment for IBS must be individualized. If you have diarrhea, treatment might include medications to bulk up your stool or slow the transit time through your bowel. If you have constipation, increasing fluid intake and dietary changes can be helpful. Using a probiotic can also be helpful, as can avoiding certain foods. If I feel that you have IBS, we’ll have a lot to discuss as we decide on treatment based on your unique symptoms.
If you have symptoms of IBS, it’s important that you come in and see me. The symptoms of IBS are similar to the symptoms of other serious conditions that should be ruled out. IBS causes real and distressing symptoms that can be treated, so make your appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Pink eye can cause discomfort, discharge from the eye and tearing. It is highly contagious, so if you think you have pink eye it is best to seek treatment, as you may pass the infection on to others, especially those in your household”.
-Dr. Bella Zimilevich, MD
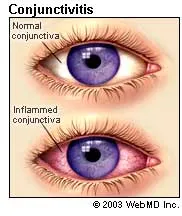
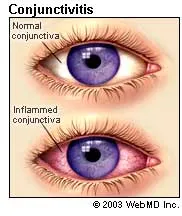
What is conjunctivitis?
The conjunctiva is the transparent membrane that covers the white of your eye and lines your eyelid. In pink eye, infection or inflammation of the conjunctiva causes inflammation of the tiny blood vessels of the conjunctiva, which results in the characteristic pink coloration of the eye. It is usually caused by infection with a virus or bacteria or by an allergic reaction.
What are the symptoms of conjunctivitis (pink eye)?
In addition to redness in one or both eyes, conjunctivitis may also cause:
- a sensation of a foreign body in the eye (gritty sensation)
- itchiness
- tearing
- discharge/crusting of the eye which is usually worse in the morning
Do I need to see a doctor if I have pink eye?
Yes. Pink eye can be highly contagious. If you get treatment as soon as your symptoms start, you may be able to prevent others around you from getting it. In addition, your symptoms may not be caused by pink eye but by another eye condition that is more serious. Eye health should always be taken seriously. If you have blurred vision and pain in one or both eyes in addition to redness, it is imperative that you seek medical care as soon as possible.
What causes pink eye?
Pink eye may be caused by the following:
- Bacterial/viral infections– if you have a viral or bacterial infection, you will likely experience copious watery discharge (viral infection) or a thick yellow or green discharge (bacterial infection) in addition to redness of one or both eyes. Infectious conjunctivitis often occurs at the same time as a cold or a respiratory illness. Viral and bacterial conjunctivitis is very contagious. It is spread by direct contact with an infected person, or by contact with items an infected person has touched (indirect contact). If you have children who have conjunctivitis it is important that you wash your hands frequently and have them do the same, and ensure that your children are treated by their doctor.
- Allergic conjunctivitis– if you suffer from allergies, your eyes may also be affected. Your eyes may be reddened and itchy and may water uncontrollably. You may also suffer from a runny nose and may sneeze frequently. Allergic conjunctivitis occurs after exposure to an allergen such as pollen.
- Foreign objects/substances in the eye– if you have inadvertently splashed a chemical in your eye or something has been blown by the wind into your eye, you will know it! Your eye will be irritated and you will feel as though you have something in your eye. Your eyes may water profusely as your eye attempts to flush out the foreign object or substance. If you think (or know) that there is something in your eye that shouldn’t be there, try not to rub your eye. Flush your eyes with saline if you have any and come to see me right away, or head to the nearest emergency room. Foreign objects or substances, particularly chemicals, may damage the eye and may threaten vision. Many workplaces in which chemicals are used have eye wash stations for these types of emergencies.
What can I expect when I come in to see you?
First of all, I will need to know how long you have had symptoms and what symptoms you are experiencing. I will also need to know if anyone you have been in contact with has similar symptoms. I will ask if you have allergies to pollen or dust that may be causing your symptoms. I will need to know if both or a single eye is affected. I will also need to know if you wear contact lenses. I will ask if you have pain in your eye(s) and whether your vision is affected.
I will examine your eye carefully. This may involve shining a light in your eye. I may also assess your vision using an eye chart. I may perform other exams as necessary, including staining the surface of your eye with a short-acting dye and viewing your eye with a slit lamp to see if your cornea has been injured.
If you have conjunctivitis caused by a bacterial infection, I may prescribe eye drops or an eye ointment. If your symptoms are caused by allergies, there are eye drops that can help. I will instruct you regarding how to instill your drops or ointment. If I am concerned that your eye problem is caused by something more serious than conjunctivitis, I may refer you to an eye specialist. In most cases, conjunctivitis clears up quite quickly.
If you have symptoms of conjunctivitis, don’t wait to come in- conjunctivitis is often very contagious and you may inadvertently spread the infection to others, so call today for your appointment.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Many people have prediabetes and don’t know it. If you have risk factors for diabetes or a strong family history of diabetes, you should be coming in to be screened routinely. Prediabetes does not necessarily guarantee that you will develop diabetes- instead, you can think of it as a wake up call to change those risk factors which can be changed before it is too late”.
-Dr. Zimilevich, MD
What is prediabetes?
Prediabetes is characterized by blood sugar levels that are abnormally high but are not yet high enough to be classified as full-blown type 2 diabetes. Untreated, prediabetes often progresses to type 2 diabetes within 10 years. Even if you do not yet have diabetes, changes may already be occurring in your heart and blood vessels as a result of even sporadically high blood sugar levels. The good news is that you can halt the progression of prediabetes to diabetes by making some lifestyle changes- diabetes does not have to be your future!
What are the symptoms of prediabetes?
Most people who have prediabetes are unaware that they have the condition, because their condition has not progressed to the point of experiencing symptoms. In fact, many people with diabetes type 2 are not aware they have diabetes until it is discovered during routine health screening.
One of the few visible signs that you are at risk of developing diabetes is discoloration of the skin. The skin in certain areas of your body may be darker than normal. Areas frequently affected include the neck, elbows, knees, knuckles and armpits (see picture).

Acanthosis nigricans, a discoloration of the skin associated with prediabetes.
Symptoms of type 2 diabetes include:
- increased thirst
- increased urination
- blurry vision
- fatigue
By the time you begin to experience these symptoms, you likely already have diabetes.
What are the risk factor for prediabetes and diabetes?
There are many situations that put you at increased risk of developing prediabetes. Some of these risk factors can be modified while others can’t.
Risk factors that cannot be modified include your age (increasing age is a risk factor for diabetes), your family history and your race (African Americans, Hispanics and Asian people are at increased risk for diabetes).
Risk factors that you can change include:
- your weight (obesity is a risk factor for diabetes)
- your activity level (a sedentary lifestyle increases your risk of becoming obese and developing diabetes)
- hypertension (having high blood pressure is a risk factor for diabetes)
- high cholesterol (if your “good” cholesterol is low and your triglycerides are high you are at increased risk)
If you are a woman and you had gestational diabetes during pregnancy you are at higher risk of developing type 2 diabetes. Also, if you have been diagnosed with PCOS (polycystic ovarian syndrome) you are at risk for developing diabetes.
What causes diabetes?
Researchers have identified specific genes associated with insulin resistance. Excess abdominal fat and lack of exercise are also implicated in type 2 diabetes.
People who have prediabetes and diabetes cannot process sugar in the same efficient way that others do. In healthy people, the pancreas secretes insulin in response to a meal or a snack. Insulin is a hormone which allows the body’s cells to use glucose for energy. In people with prediabetes and diabetes type 2, their bodies cannot use insulin as effectively, so that sugar builds up in the bloodstream instead of being used by the cells that require glucose to do their jobs (in type 1 diabetes, the pancreas does not secrete insulin at all, or secretes very little).
How do I know if I should be screened for prediabetes?
If you have any of the risk factors listed above, you are at risk of developing prediabetes. You should make an appointment to come in and see me so that we can assess your level of risk and determine how often you should be screened. We can also discuss what you can do to decrease your risk, including weight loss, exercise and management of high blood cholesterol and high blood pressure. By successfully managing your risk factors, you can significantly reduce your risk of developing diabetes.
What should I expect when I come in to see you?
When you come in to see me, I will first need to gather some information. I will need to know about your past medical history if you are a new patient. I will also need to know if you are taking any medications and if you have any allergies.
Next, we’ll explore your personal risk factors. I may weigh and measure you and so that I can determine your BMI (body mass index- a standardized scale combining height and weight that helps to determine amount of body fat). I will take your blood pressure. I will ask you about other risk factors you may have (i.e. gestational diabetes, family history of diabetes). I will ask you about your diet and exercise patterns. I will also want to know whether you have symptoms of diabetes (increased thirst and urination, fatigue, vision changes).
Screening will involve some diagnostic testing, including a fasting blood glucose level and cholesterol testing. I may order other tests depending on your results and whether you have any other health conditions.
Once I have gathered all the information I need, I will have you return to see me so that we can discuss your results. If your blood glucose is normal but you have risk factors for prediabetes, we can talk about ways to reduce your risk. If your blood glucose is found to be high and you have prediabetes or diabetes type 2, we will discuss how to manage this.
If you are at high risk for developing diabetes, it is important to be screened regularly and to find a physician that you can work with to decrease your risk and modify those risk factors which can be modified. I would love to partner with you to help you avoid developing diabetes, or to manage your condition if you have it. Please call to make your prediabetes screening appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Shingles is an extremely painful condition that can result in a chronic pain syndrome called postherpetic neuralgia. If you think you may have shingles it is important to seek help. Antiviral medication given in the first few days can reduce the risk of neuralgia. Don’t wait if you have symptoms of shingles- make an appointment right away and come in to see me”.
-Dr. Zimilevich, MD
What is shingles?
Shingles is a reactivation of the same virus that causes chickenpox (varicella zoster virus). Once you have had chickenpox, the virus goes dormant, hiding in the nerve tissue surrounding your brain and spinal cord. Many years later, the virus can reactivate, causing the condition known as shingles. Although shingles is more common after age 60, people of any age can get shingles if they have had chickenpox. The condition is very common, affecting almost 1/3 of the population at some point in their lives. You should know that although shingles is caused by a type of herpes virus, it is not the same herpes virus that causes genital herpes, the sexually transmitted infection.
What are the symptoms of shingles?
Pain is often the first symptom of shingles and may occur before the rash makes its appearance. The pain is often described as burning in nature. Skin in the affected area may be hypersensitive, so that even clothing rubbing against the area will be painful. The pain may precede the rash by several days to a week.
When the rash appears, it will look like tiny blisters on top of a reddened base. New blisters may continue to form for up to 5 days. The rash follows a dermatome (the path of an individual nerve as it comes out of the spinal cord), creating a band-like pattern. The rash usually occurs on only one side of the spinal cord. Rarely, more than one nerve will be affected, but usually a single nerve is affected.
The blisters eventually rupture and they will ooze and crust before they heal, much like chickenpox. The condition may last 3 to 4 weeks from the beginning symptoms until resolution of the rash.
Is shingles contagious?
Yes, but not in the way you might think! People who have shingles can pass the virus on to individuals who have never had chickenpox, or who have never been vaccinated for chickenpox, and these unlucky people will get chickenpox, not shingles. They may develop shingles at a later time, but they won’t get shingles from contact with someone who has it.
Can shingles cause complications?
Yes. Although most people with shingles recover completely, complications sometimes occur. Shingles may affect the eye when nerves of the face are involved. This can be very serious and may lead to vision loss. Hearing can also be affected, as can the facial nerves, leading to facial paralysis on the affected side.
The most dreaded (and most common) complication of shingles is postherpetic neuralgia, in which the pain of shingles lingers long after the rash has subsided. The pain can be severe and debilitating. This is why it is important to seek help immediately if you suspect you may have shingles, as treatment with antiviral medications in the first 72 hours of symptoms may reduce the risk of this devastating complication.

Is there a vaccine for shingles?
Yes. There is a vaccine for adults over the age of 50 who have had chickenpox. The vaccine has been found to reduce the occurrence of shingles and significantly reduces symptoms, including the incidence of postherpetic neuralgia. If you get the vaccine and still develop shingles, you will likely have a much less severe case.
What can I expect when I come in to see you?
If you come in to see me with symptoms of shingles, I will first need to know a little about your past medical history. I will also want to know what medications you are taking and if you have any allergies to medications. I will want to know if you have any medical conditions that affect your immune system (and thus your ability to fight off infection).
I will ask you when your symptoms started. If you have pain, where is the pain located and when did it start? Does the pain come and go? What is the character of the pain? Is it sharp, stabbing, dull, aching or something else? Is there anything that makes the pain better or worse?
If you have a rash, I will need to examine your rash. I will look for the tell-tale blisters along a nerve distribution, which is characteristic of shingles.
Usually your symptoms, along with the characteristic appearance of your rash, is enough to make the diagnosis. If I believe that you have shingles and it has been less than 72 hours since your symptoms started, I will prescribe an antiviral medication. The medication will lessen the severity of your symptoms and hopefully shorten the duration of symptoms. If you have shingles on your face that may affect your eye, I may send you to an eye specialist.
If you have symptoms of shingles, you should make an appointment to see me immediately. Diagnosing and treating shingles as soon as symptoms start is the best way to limit the symptoms of this painful condition.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Almost everyone vomits from time to time. Brief episodes of vomiting may be due to a virus or a dietary indiscretion. For some people, vomiting occurs as part of a pattern of illness. If you are vomiting frequently or have other warning signs of a serious illness, it’s important that you seek medical care.”
-Dr. Zimilevich, MD
What is the difference between nausea and vomiting?
Nausea is the sensation that you are about to vomit. It may occur by itself or may actually be followed by vomiting, which is the forceful ejection of the stomach contents up through the esophagus and out your mouth. Both nausea and vomiting are extremely unpleasant sensations that most people would just as soon avoid!
Causes of nausea and vomiting
There are many conditions that can make us feel nauseated or cause us to vomit. The following is only a partial list:
- stomach or intestinal infection with a virus or bacteria– we’ve all experienced “the stomach flu”, which often causes nausea, vomiting and diarrhea for a day or two and usually subsides on its own without treatment. Viral gastrointestinal illnesses are extremely contagious and can be passed from person to person very easily. Bacterial illness affecting the GI tract may result from eating contaminated food (“food poisoning”) and can make you feel very ill. Food poisoning often requires medical treatment.
- acid reflux and GERD (gastroesophageal reflux disease)- in GERD, patients sometimes vomit because the flap of tissue between the stomach and esophagus which prevents food from “refluxing” from the stomach back up into the esophagus is incompetent
- pain– patients will sometimes become nauseated when they are in pain and may actually vomit when pain is severe (think kidney stones and migraine headaches)
- food intolerance/allergies– some people become nauseated when they eat foods that they are sensitive or allergic to, or foods that they lack the proper enzyme to digest
- medications– many medications, such as antibiotics and opioids, have nausea as a side effect (which doesn’t necessarily mean that the person is allergic to the medication); nausea due to medication may pass as your body adjusts to the medication
- motion sickness– some people become nauseated and may vomit when they travel by car or boat
- morning sickness- some women experience nausea and vomiting during pregnancy, thought to be due to hormonal changes
- ulcers– some people with gastric or duodenal ulcers may experience nausea/vomiting
- bowel obstruction– nausea and vomiting are common symptoms of bowel obstruction, more typically with small bowel obstructions
- cancer or cancer treatment– certain types of cancer may cause nausea and vomiting (i.e., colon cancer resulting in bowel obstruction); chemotherapy, radiation and other cancer treatments may also cause nausea and vomiting
How do I know if I need to be seen by a doctor?
As can be seen, nausea and vomiting may be caused by a number of conditions, some fairly benign and others far more serious. It can be difficult to determine when you should come in to be assessed. The following are some guidelines:
- dehydration- if you are unable to keep any fluids down, or you are vomiting very frequently and/or experiencing diarrhea, you may become dehydrated. If you are dehydrated, you may feel weak, dizzy and very thirsty with a dry mouth. You may urinate less often, your urine may appear darker than normal and your eyes may appear sunken in your eye sockets. Even a simple virus can cause significant dehydration that can be dangerous, especially if you have an underlying health condition. If you have been vomiting for longer than a day, or have been unable to keep any fluids down for longer than 12 hours, it may be time to seek help.
- abdominal pain– if you are experiencing severe abdominal pain along with your nausea and vomiting, this may be a sign of a more serious condition such as a bowel obstruction, especially if you are not passing flatus (gas) and have not had a bowel movement in some time.
- urination– if you are urinating infrequently, your urine is very dark in color or you have not voided in longer than 8 hours, you are likely dehydrated.
- vomiting blood– if you are vomiting blood, or dark material resembling coffee grounds, you should seek emergency care
- fever– you may experience a low-grade fever with viral gastrointestinal illness; if your fever is over 101 degrees Fahrenheit you should seek medical care
- weight loss– if you have been nauseated and/or vomiting for a prolonged period of time you may lose weight, which could signify a serious problem.
These are guidelines only. If you are feeling very sick, you should seek medical care- you do not need to have any or all of these symptoms!
What can I expect when I come in with nausea or vomiting?
When you come in to see me complaining of nausea and vomiting I will first need to ask you about your past medical history, any medications you are taking and whether you have any allergies to foods or medications.
Once I have gathered this information, I’ll ask you to describe your current symptoms: when they started, how many times you have vomited and whether you are also experiencing diarrhea or other symptoms such as abdominal pain or fever. I will also ask whether you have taken any over-the-counter remedies for nausea and vomiting and whether they were helpful. I’ll ask you to estimate your fluid and food intake. Once I have gathered all of the pertinent information I will examine you, focusing on signs of dehydration and your abdomen. I will listen to your abdomen and feel for any masses or tender areas that may provide clues as to the cause of your symptoms.
If necessary, I will order lab work such as a CBC and electrolytes to help me determine your level of dehydration and whether an infection might be causing your symptoms. If you are also suffering from diarrhea, I might order a stool culture to look for bacteria in your stool. I may also order an abdominal x-ray if I feel it is needed based on your symptoms.
Once I have gathered the information I need we’ll sit down and discuss what I think is causing your symptoms of nausea and vomiting. Together we’ll decide on the best course of action.
If you have been experiencing nausea and vomiting for longer than a day or two, especially if you are unable to keep fluids down, make an appointment to come in and see me. Whether it takes one visit or more, we’ll figure out what the problem is and get you feeling better!
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“An abscess can be quite painful and may be unlikely to heal on its own. Making a small incision and draining the contents can provide relief of pain and speed healing. If you have a painful abscess, make an appointment to see me urgently”.
-Dr. Bella Zimilevich, MD
What is an abscess?
An abscess is a collection of pus under the skin. It is caused by a bacterial infection and often forms at the base of a hair shaft or around a blocked sweat gland. It may also occur from a small injury to the skin. In an abscess, white blood cells rush to the affected area to fight the bacteria causing the infection. Pus is a conglomeration of damaged tissue debris and white blood cells. An abscess may contain quite a large amount of pus.
What are the symptoms of an abscess?
If you have an abscess, the first thing you might notice is pain. Abscesses can be quite tender. They may appear as a large pimple-like lump with a domed peak. The skin around it may be red and warm. The abscess itself may feel firm. You may notice pus coming from it if it has opened. You may develop fever and chills, depending on the size and location of the abscess. Abscesses can form anywhere.

Does an abscess need to be treated?
If your abscess has burst and is draining on it’s own and you do not have fever, you can watch the abscess for a day or two to see if it is going to resolve on its own. You should never squeeze or milk the pus from an abscess! Keep the area clean and dry.
Most abscesses will not clear up so easily and will require medical care. Left untreated, you may feel quite ill and the pain may cause you to seek care. It’s best to see a doctor for your abscess, as incision and drainage, followed by antibiotics, is often needed.
What can I expect when I come in?
When you come in to see me, I will first need to know a little about you, such as whether you have any chronic health conditions, whether you are taking any medications and whether you have any allergies.
I’ll need to take a look at the affected area. You may be asked to change into a gown, depending on the location of your abscess. I’ll examine the area to make sure that it is an abscess and not another problem. I’ll ask when it appeared, whether you have had one before and whether you have had any fever or chills.
Incision and Drainage
There’s a very good chance that I will need to drain your abscess if it is large and painful. Doing so will relieve pain and speed the healing process. Incision and drainage involves the following:
- cleansing of the skin over the abscess with an antiseptic agent
- freezing of the area using a local anesthetic
- making an incision over the top of the incision from top to bottom
- expressing the abscess to encourage drainage
- exploring the abscess to ensure I have gotten all of the infected material out (for larger abscesses)
- packing the abscess to prevent the wound edges from healing together (for larger abscesses)
- applying a dressing to the area to soak up any further drainage
The entire procedure lasts only about 10 minutes for an uncomplicated abscess. The abscess is left open to allow it to drain and heal. Suturing it closed may result in further infection. You may be asked to return the next day if I packed your abscess- when you return I will remove the packing and recheck the wound.
I may prescribe antibiotics depending on how large the abscess was, whether you have fever and what I believe the causative agent is. Most simple abscesses are caused by Staphylococcus or Streptococcus, common organisms that live on your skin and only cause infection when they manage to make their way under the skin through a small break. If I prescribe antibiotics, it is important that you take them as directed and finish the entire course.
In some cases, I may elect not to drain your abscess and send you to a specialist. This may occur if your abscess is very large or in an area that I feel is particularly delicate (such as near the genitals or rectum). If this happens, I will explain why it is best that you go elsewhere for care.
If you have an abscess that is reddened, swollen and painful, make an appointment to come in and see me. In most cases, an abscess will not heal without medical care. Medical care can ease the pain and speed healing. In most cases, I will be able to get you in quickly, so call today to make your appointment.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Pneumonia is usually caused by a virus or a bacteria and can make you feel very ill, particularly if you have underlying heart disease, diabetes or lung disease such as asthma or COPD. In people with chronic health conditions, weakened immune systems or the elderly, pneumonia can be life-threatening if left untreated. If you think you may have pneumonia, you should make an appointment to come in immediately”.
-Dr. Zimilevich, MD
What is pneumonia?
Pneumonia is an infection of the lungs. In pneumonia, the tiny air sacs that are responsible for gas exchange fill up with fluid and/or pus. This causes congestion of the lungs and is responsible for the coughing that is prominent in pneumonia. It may also cause difficulty breathing. Anyone can get pneumonia, but people with weak immune systems, the elederly and the very young are most at risk from this always serious and sometimes deadly disease.
What are the symptoms of pneumonia?
If you have pneumonia, you will usually feel quite ill and may feel sicker than you do when you have a cold. Symptoms may include:
- productive cough
- fever/chills
- chest pain
- difficulty breathing/shortness of breath
- decreased appetite
- sore throat (may be due to coughing)
- headache
- fatigue
- body/muscle aches
- GI upset (nausea/vomiting, diarrhea
- decreased level of consciousness (in the very ill)
- lower than normal body temperature (in the elderly or people with weak immune systems)
What causes pneumonia?
Pneumonia can be caused by bacteria, viruses or fungi. If you are healthy and young, your immune system can normally prevent microorganisms from invading your lungs, but if you are older, have a chronic health condition or your immune system is not up to snuff (i.e. you are being treated for cancer or your body is fighting another infection somewhere else) you may be at higher risk for pneumonia.
Pneumonia may occur on its own, or it may occur after you have had a cold or the flu as a secondary infection. This is why it is so important to get an annual flu shot– not only does it prevent the flu, but it can also stop you from developing a secondary pneumonia, which can be very serious when your immune system is exhausted from fighting the flu.
Pneumonia that occurs when you have been in the hospital for another reason is called hospital-acquired pneumonia. This type of pneumonia can be more difficult to treat than pneumonia that is community-acquired.
What can you expect when you come in to see me ?
When you come in to see me, I will want to know a little about your history (if you are a new patient). I will need to know if you have any health problems and whether you are taking any medications. I will also need to know if you are allergic to any medications.
I’ll ask you when your symptoms started. Have you had a cold or the flu? What symptoms are you experiencing? Does anything make them better or worse? Tell me as much as you can about your symptoms and how you have been feeling.
Once I have gathered some information, I’ll want to examine you. I will look in your ears and throat and feel your neck for swollen glands. I’ll listen carefully to your heart and lungs for abnormal breath or heart sounds. I may also examine your abdomen.
Based on my findings, I may order diagnostic tests such as a chest x-ray and blood work to look for signs of bacterial infection and perhaps dehydration.
Once I have all the information I need, we’ll discuss the results of my examination and any tests I may have ordered. If I believe you have pneumonia caused by a bacteria, I will prescribe antibiotics. If I order antibiotics it is important that you finish the entire course of antibiotics. If you are not better in a few days after starting your antibiotic, you should come back in to see me. If you have a viral pneumonia, antibiotics will not be helpful.
Other things you can do to speed your recovery include:
- drinking plenty of fluids (this helps to thin out the secretions in your lungs)
- get plenty of rest
- eat as healthily as you can
- manage your fever and muscle aches with an over-the-counter pain medication
- avoid smoking or being around people who smoke
{Note: if you are experiencing severe chest pain or shortness of breath, you should go to your nearest emergency room}
If you think you have pneumonia, you should not wait to be seen. Pneumonia is a very serious condition and can be life-threatening for the elderly, people with chronic health conditions and people whose immune systems are compromised. If you have symptoms of pneumonia, make an appointment now to come in and see me.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Most women will experience a yeast infection at some point in their life. Yeast infections are very common and are not a sexually transmitted disease. They can be easily treated. If you have symptoms of a vaginal yeast infection and aren’t sure about your symptoms, come in and see me.”
-Dr. Bella Zimilevich, MD
What is a vaginal yeast infection?
Vaginal yeast infections cause irritation of the vagina and vulva (the tissue surrounding the vagina). It is a very common infection- almost all women will experience at least one yeast infection in their life. For some women, yeast infections may occur more than once.
What causes vaginal yeast infections?
Yeast infections are caused by an overgrowth of Candida albicans. Candida is always present in the vagina, but sometimes an overgrowth of this yeast occurs, resulting in the symptoms of yeast infection. Overgowth can occur when the pH of the vagina is altered. Many factors can influence the internal conditions of the vagina, including:
- hormonal changes– some women may experience a yeast infection around the time of their period due to hormonal changes; pregnancy also increases the risk of developing a yeast infection
- illness
- medications– steroids and birth control pill may increase your risk of infection; antibiotics are the worst offenders because they kill of the normal flora (healthy bacteria that reside in the vagina) that normally keep yeast in check
- altered immunity– conditions such as HIV and diabetes can make your body more prone to yeast infections
- lifestyle factors– stress, lack of sleep and a poor diet have all been implicated in yeast infections

What are the symptoms of a yeast infection?
Symptoms of a yeast infection may include:
- redness and swelling of the vagina and vulva
- soreness/itchiness of the affected area
- pain during intercourse or when urinating
- a rash in the vaginal area
- thick, white discharge the consistency of cottage cheese but without an odor
Symptoms can be mild or very severe. If your symptoms are very severe, you will be unlikely to be able to ignore them.
Do I need to see you if I think I have a yeast infection?
It depends. If you have never had a yeast infection before, you should come in and see me. Yeast infection symptoms can be similar to the symptoms of certain sexually transmitted infections. It is best to be sure you actually have a yeast infection.
If you have had a yeast infection before and you are in a monogamous sexual relationship (meaning that you are fairly certain that both you and your partner have not been with anyone else), you might try an over-the-counter remedy recommended by your pharmacist.
If you treat yourself and your symptoms do not improve or they reoccur, you need to come in and see me.
What can I expect when I come in to see you?
When you come in and see me, I’ll ask you about any health problems you might have. I will also ask about any allergies you have. I’ll ask when your symptoms started and whether you have had similar symptoms before (and if so, how were you treated?)
In order to make the correct diagnosis, I will need to examine you. You will be asked to change into a gown and provided with a sheet for comfort and modesty while I examine you. The entire procedure is over in minutes and is not painful; although it may be mildly uncomfortable if you are inflamed in the vaginal area. I’ll explain everything I am doing before I do it, and if you are feeling nervous, or if you have never been examined before, please feel free to ask questions or let me know. I’ll tell you what to expect every step of the way.
If I think you have a vaginal yeast infection, I may prescribe an antifungal cream or suppository. I may also prescribe an oral antifungal medication. What I prescribe will be dependent on whether this is your first yeast infection and your overall health.
If you have had frequent yeast infections, I may suggest treating your partner as well. Although a yeast infection is not a sexually transmitted disease, men can also get a yeast infection and it is possible that you and your partner may pass the infection back and forth to each other. In addition, I may do some testing to make sure that your immune system is functioning the way it should.
Can yeast infections be prevented?
There are several things that you can do to avoid a yeast infection. Yeast thrives in a warm and moist environment, so bearing that in mind:
- avoid douching (this may kill off the normal flora of your vagina, allowing yeast to overgrow)
- avoid tight clothing or underwear made of nylon or synthetic fibers that don’t “breathe”
- shower instead of bathe, and avoid hot tubs
- get out of your wet bathing suit as soon as possible
- avoid bubble baths and other scented products that come in contact with the vaginal area
If you think you have a yeast infection but aren’t sure, or you are experiencing frequent yeast infection, make an appointment to come in and see me. We’ll soon have you feeling back to normal.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Rheumatoid arthritis differs from osteoarthritis in that it not only causes joint pain and stiffness, but can also affect other body systems. RA often affects younger adults, which can impair ability to work. If you have joint pain and stiffness, regardless of your age, you should come in and see me- there are treatments that can help”.
Dr. Zimilevich, MD
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is an autoimmune disorder in which the body attacks itself- usually the small joints of the hands and feet, although any joint may be affected by RA. It is the most common type of autoimmune arthritis. Women are affected more often than men (3:1). It is estimated that over 1 million people in the US are living with RA, many of them relatively young. Rheumatoid arthritis most often affects people in their 40s, 50s and 60s, but it can occur at any age (when the disease is diagnosed in children it is called juvenile arthritis)
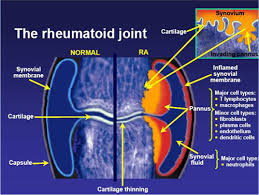
What are the symptoms of rheumatoid arthritis?
The joint pain of RA is often at its worst in the morning when you first wake up. You may find it difficult to move the affected joints well and without pain when you first wake up. The pain may improve as the day wears on; as the disease progresses, or during acute flares of the disease, pain may be constant.
Because RA is an autoimmune disease, other organs of the body may be affected as well. You may also experience:
- loss of appetite
- fever
- fatigue
- dry eyes and mouth
- rheumatoid nodules (firm mobile lumps that grow under the skin in the hands, elbows)
- lung problems
- anemia (low number of red blood cells)
What causes rheumatoid arthritis?
While experts understand that RA is an autoimmune disease, no one knows what triggers the immune system to attack the synovial membrane of a joint. The synovial membrane is the tissue that lines the joint. The immune system releases chemicals that attack this lining, as well as the cartilage that cushions the joints and the joints themselves. It is likely that some people are genetically susceptible and the disease is triggered by an unknown event.

What can I expect when I come to see you?
If you suspect that you may have RA, it is best to come see me as soon as possible. Early treatment can help prevent disease progression, and RA requires constant monitoring to prevent destruction of joints.
I will start off by taking a history from you. I’ll need to know about your past medical history, medications you are currently taking and any allergies you may have. I will then ask you to tell me about your symptoms: when did they start, when is the pain at its worst and what makes the pain better or worse. I may also ask whether you have noticed any fever, excessive tiredness or other constitutional symptoms.
Once I have learned more about your symptoms, I will want to examine your joints, particularly the joints of your wrists, hands and feet. I will look at your other joints as well. I will be looking for redness, swelling and warmth, as well as pain with manipulation of the joints.
Unfortunately, there is no single test I can order that can tell me whether or not you have arthritis, but there are blood tests that can provide clues. If I suspect you may have RA, I might order numerous blood tests that may provide supporting evidence to the diagnosis. These blood tests might include:
- complete blood count- to check for anemia
- rheumatoid factor- a protein found in the blood of many people with RA (although not all)
- erythrocyte sedimentation rate- a non-specific marker for inflammation which can be elevated in many conditions including RA
- anti-CPP- blood test to look for antibodies to certain peptides found in the blood of some people with RA
Although x-rays may not be helpful in the early stages of RA, they can be used to mark the progress of the disease. X-rays in the first months of RA may appear normal, but that does not mean you don’t have RA.
Can you treat me?
I am an internal medicine physician with a specialty in geriatric medicine. I can help you manage your disease. If necessary, I would refer you to a rheumatologist to confirm your diagnosis and make treatment recommendations. Many people see a rheumatologist periodically and depend on their primary care doctor to manage their condition the rest of the time. It can be difficult to get in to see a specialist when needed- for this reason, you will need a physician you can depend on to treat you between visits to a specialist. I would love to partner with your rheumatologist to help you with your condition.
Today, there are many treatment options for RA. Medications can help you live a relatively healthy and normal life and can induce remissions in the active disease process. If you think that you may have RA, it is important that you receive a proper diagnosis and begin treatment to prevent worsening of the disease. Make your appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.

“Psoriasis symptoms can be mild and more of a nuisance than anything, or it may be severe and disabling. It can also be a major cosmetic concern. If you think you may have psoriasis, treatment is available to improve your symptoms and the appearance of your skin”.
-Dr. Zimilevich, MD
What is psoriasis?
Psoriasis is a chronic disease which causes the skin cells to build up very rapidly, resulting in red, dry and itchy patches that can be quite sore, or thick silvery-colored scales. The disease may have periods of remission during which symptoms are almost non-existent, alternating with periods in which you have a “flare” of symptoms. The condition is often associated with arthritis. When arthritis is present, symptoms can be quite severe.
What are the symptoms of psoriasis?
- dry and cracked skin that is prone to bleeding
- itching or burning areas of the skin
- small spots that form scales
- reddened patches of skin that may eventually form silvery-colored scales
- pain and stiffness in the joints
- discoloration, thickening and/or pitting of the nailbed
As mentioned, these symptoms may be relatively mild or severe, and symptoms may come and go.
What causes psoriasis?
No one fully understands what causes psoriasis. It is believed to be an autoimmune disease, meaning that the body attacks itself- in this case, the body attacks the skin. It seems that some people are genetically susceptible to psoriasis. It is possible that elements of the environment also play a role in psoriasis.
Our body contains cells called T cells. T cells are responsible for helping us to fight off infections. In psoriasis, the T cells mistakenly target the skin and cause skin cells to build up far too quickly. Normally it takes weeks for a skin cell to move to the outermost layer of the skin where it can be shed. In psoriasis, skin cells are created more quickly, and they also travel to the outer layer of the skin too quickly, where they build up into scales on the surface of the skin. What causes the T cells to malfunction is somewhat of a mystery.
Triggers for psoriasis
If you have psoriasis, certain things may cause the disease to flare, or make your symptoms worse:
- an injury to the skin, such as sunburn or a skin infection
- medications such as blood pressure medications, iodides and lithium (used to treat a mental health condition known as bipolar disorder)
- exposure of the skin to the cold/cold weather
- alcohol consumption (in large amounts)
- smoking
- infections (thrush, strep throat)
Are there complications associated with psoriasis?
Yes. If you scratch affected skin, you may develop a bacterial skin infection. If you have psoriatic arthritis, your joints may eventually become damaged.
Possibly the worst part about having psoriasis for many people is the cosmetic aspect of the disease. People with severe psoriasis may have low self-esteem due to their feelings about their appearance. This may lead to stress, anxiety and depression. Some people with severe psoriasis may even isolate themselves because of how they feel about their appearance.

What can I expect if I come in for an appointment?
If you think that you may have psoriasis, you should make an appointment. You need a proper diagnosis before any treatment can be prescribed.
When you come in to see me, I will want to know about your past medical history, any allergies you have and what medications you are currently taking (if any). I will also want to know when you began experiencing symptoms, whether your symptoms are continuous or seem to come and go and what (if anything) makes your symptoms worse or better.
Once I have obtained your history, I’ll take a look at the affected area(s) of skin, looking for redness, dryness, cracking of the skin, weeping, crusting and other signs and symptoms. Psoriasis can sometimes look like other skin conditions such as atopic dermatitis, so I will need to look closely.
Treatment of psoriasis
Treatment of psoriasis may include creams or ointments applied to the skin, oral or injected medications and light therapy.
- creams/ointments (topical therapy)– if you have mild to moderate psoriasis, a medicated cream or ointment may control your symptoms and provide relief. Topical steroid creams, retinoid creams and coal tar are common topical therapies used to treat psoriasis.
- oral/injected medications– these treatments are used for moderate or severe psoriasis, especially if arthritis is present. These medications can cause serious side effects, so they may be used in short bursts or combined with other therapies.
- light therapy (phototherapy)– psoriasis may be treated with natural or artificial ultraviolet light; phototherapy may be combined with medication to increase effectiveness
If you think you have psoriasis, your first step is to make an appointment to come in and see me, particularly if you also have signs and symptoms of arthritis. I will work with you to get you a proper diagnosis. If necessary, I will refer you to a dermatologist. Psoriasis needs ongoing treatment and close monitoring to prevent complications. Make your appointment today.
Our Location

6301 Mill Lane, Brooklyn, NY 11234.



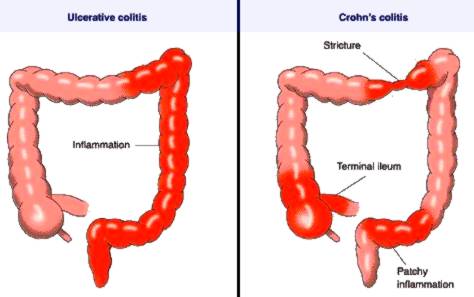

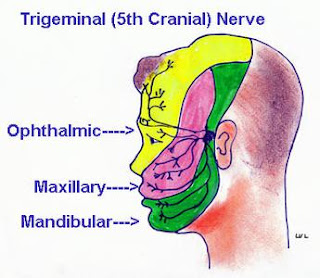

 stable angina– unstable angina occurs not only during activity, but also at rest. Unstable angina is unpredictable and may not stop when you rest or take medication. Unstable angina is a warning that a heart attack may be imminent and should be taken very seriously.
stable angina– unstable angina occurs not only during activity, but also at rest. Unstable angina is unpredictable and may not stop when you rest or take medication. Unstable angina is a warning that a heart attack may be imminent and should be taken very seriously.